Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Idiopathic Inflammatory Myopathy (IIM) – comprising polymyositis (PM), dermatomyositis (DM), and inclusion body myositis (IBM) – is rare and difficult to study. We sought to study its’ epidemiology in the US veteran population – an understudied area.
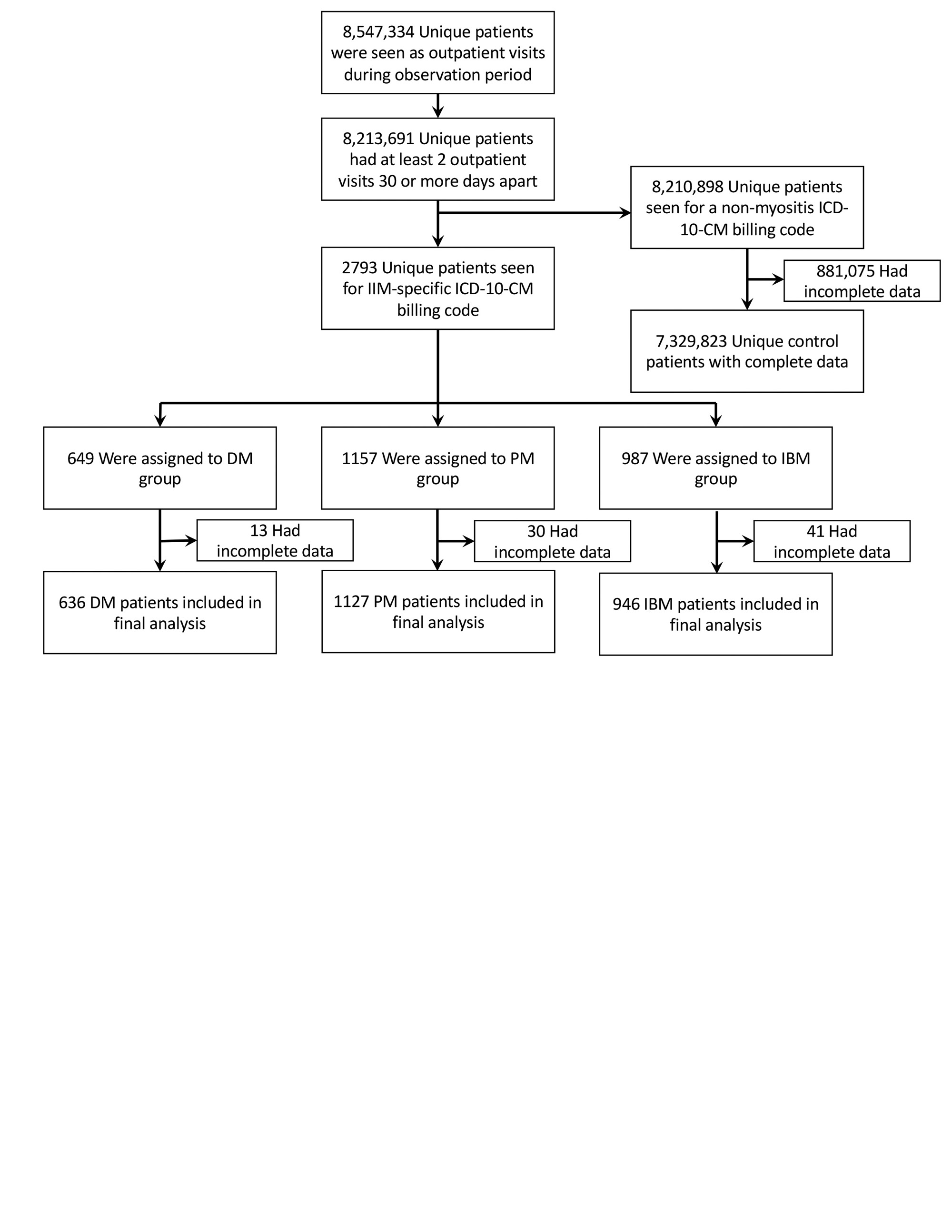
Methods: We conducted a retrospective case-control analysis using the Veterans Affairs Corporate Data Warehouse. Cases were identified based on billing data: adults aged 18 to 110, seen between 1/1/2016 and 12/31/2021, with a minimum of two visits denoted by an IIM-specific ICD-10 code. Interstitial Lung Disease (ILD) and oncological comorbidities were identified similarly. DM, PM, and IBM cohorts were randomly matched with age-, sex-, and ethnicity-paired controls on a 3:1 basis. The primary outcome examined was all-cause mortality with secondary outcomes examining the impact of age, sex, and presence of ILD and oncological diagnoses on IIM patient survival.
Results: Complete data was available for 636 DM, 1127 PM, and 946 IBM patients (Figure 1). Calculated prevalence was 79.0 cases of DM/million, 140.9 cases of PM/million, and 120.2 cases of IBM/million. Male:female ratios were lowest for DM at 0.4, intermediate for PM at 0.8, and highest for IBM at 4.2. IBM was the highest prevalence IIM in veterans over 65 (198.5 cases/million). Age-adjusted prevalence was 65.7 cases of DM/million, 91.7 cases of PM/million, and 45.1 cases of IBM/million for individuals over 15. Estimated average annual incidence was 11.8 cases/million for DM (range: 6.1 – 15.4), 13.3 cases/million for PM (range: 4.4 – 20.1), and 12.9 cases/million for IBM (range: 7.4 – 17.7).
The mean age of DM patients (65.0±13.5 years) was similar to the non-IIM VA population (65.1±17.2 years, p = 0.15), while the mean ages of PM (68.2±11.9 years) and IBM (75.1±8.9 years) patients were higher (p < 0.0001 for both) (Table 1). PM had the highest proportion of Black patients (429, 37.2%), with DM (155, 23.9%) also above the non-IIM veteran population (1,296,904, 17.3%, p < 0.0001 for both). IBM did not show a significant difference in racial makeup (156, 15.8%, p = 0.31).
In terms of comorbidities, only 0.7% (51,158) of the non-IIM VA population had an Interstitial Lung Disease (ILD)-associated ICD-10 code compared to 15.2% (97) of DM, 15.4% (178) of PM, and 2.8% (28) of IBM patients (p < 0.0001 for 3 pairwise comparisons). 12.6% (940,933) of non-IIM veterans had an oncological diagnosis, which was significantly lower than rates seen in either IIM group (134, 21.1%; 220, 19.5%; and 189, 20.0% for DM, PM, and IBM respectively, p < 0.0001 for 3 pairwise comparisons).
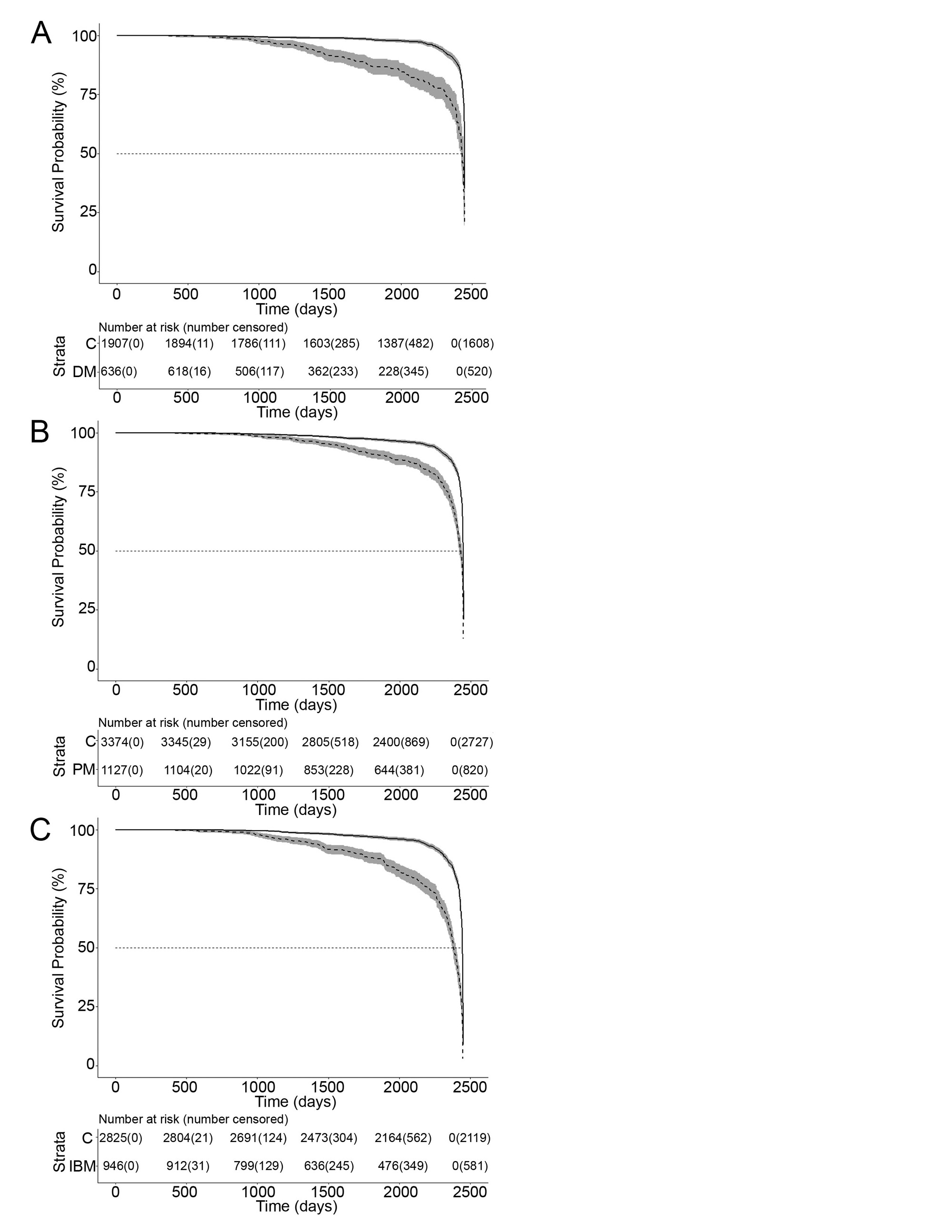
Mean (±SD) survival was 1614.2±620.9 for DM (p < 0.0001); 1901.3±563.4 for PM (p < 0.0001); and 1789.8±628.2 days for IBM (p < 0.0001) versus matched controls (Figure 2). Male sex (HR 2.6, p < 0.017), older age (HR 2.2, p < 0.001) and concurrent oncological diagnosis (HR 2.3, p < 0.001) were associated with worse survival in DM while older age was the only factor for PM (HR 2.44, p < 0.001) and IBM (HR 1.59, p < 0.001) patients. COVID infection or suspected infection had no statistical effect on survival.
Conclusion: All IIMs exhibited decreased survival compared to matched controls. Male sex and concurrent oncological diagnosis were unique poor prognostic factors in DM.
To cite this abstract in AMA style:
Liarski V. Epidemiology and Retrospective Case-Control Analysis of IIM in the US Veteran Population [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/epidemiology-and-retrospective-case-control-analysis-of-iim-in-the-us-veteran-population/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-retrospective-case-control-analysis-of-iim-in-the-us-veteran-population/