Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Multimorbidity
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is the most common chronic inflammatory arthritis, affecting 1-2% of the population. Estimates of the incidence of RA in patients with HIV (PWH) are sparse, as are data regarding the presentation of RA in PWH.
Methods: Patients were selected from the Veterans Aging Cohort Study, a longitudinal cohort of Veterans with HIV and age, sex, race, and site-of-care-matched 1:2 to uninfected Veterans. Between 1997-2017, we searched all International Classification of Diseases (ICD) codes starting from each patient’s first entry into the medical record, or in cases of PWH, from the time of diagnosis of HIV. We identified patients with ≥1 outpatient rheumatology clinic ICD code for RA and a positive or negative rheumatoid factor (RF) or anti-CCP antibodies. Charts were reviewed using the 2010 RA Classification Criteria; a score of ≥6 was classified as incident RA if there was no evidence of prior diagnosis, such as listing of RA as past medical history. We recorded conventional and biologic disease-modifying anti-rheumatic drug (DMARD) use, and reasons for changes in therapy during the first contiguous course of therapy (period with no interruption greater than 6 months).
Results: We included 56,250 PWH and 116,944 uninfected persons over 2,384,541 person-years. Of 2,748 patients with an ICD code for RA, 1,030 (37%) had at least one rheumatologist-generated ICD code and 881 (32%) had serology available. “Definite” incident RA was identified in 215 cases, 21 of whom were PWH at the time of RA diagnosis. The crude incidence of RA was 0.33 cases per 10,000 person-years (95% CI, 0.21-0.51) in PWH vs. 1.11 (0.96-1.28) in patients without. The incidence rate ratio of RA in PWH vs. uninfected was 0.29 (95% CI 0.19-0.48, p< 0.0001). Among PWH with incident RA, the median CD4 count closest to diagnosis was 487 cells/mm3 (25th-75th percentile, 367-650), and 81% of patients with recent HIV-1 viral titers available had levels less than 500 copies/mL. Most patients (88%) with incident RA were seropositive. However, high antibody titers were found less frequently in PWH: 5% of PWH had both a high (≥3 times upper limit of normal) anti-CCP titer and a high RF titer, compared to 41% of persons without HIV (Table). DMARDs were prescribed for 71% of PWH with “definite” RA, compared to 94% of uninfected Veterans (p=0.0002). The most commonly used DMARD among PWH was HCQ (57%) while methotrexate was more common in uninfected Veterans (66%). PWH were significantly less likely to be prescribed methotrexate (33% vs. 66%, p=0.004), leflunomide (0% vs. 12%, p=0.01), and biologic or small molecule drugs (10% vs. 32%, p=0.02).
Conclusion: Incident RA was less common in PWH than in matched uninfected persons. PWH with incident RA were less likely to have strongly positive autoantibody profiles than uninfected individuals.
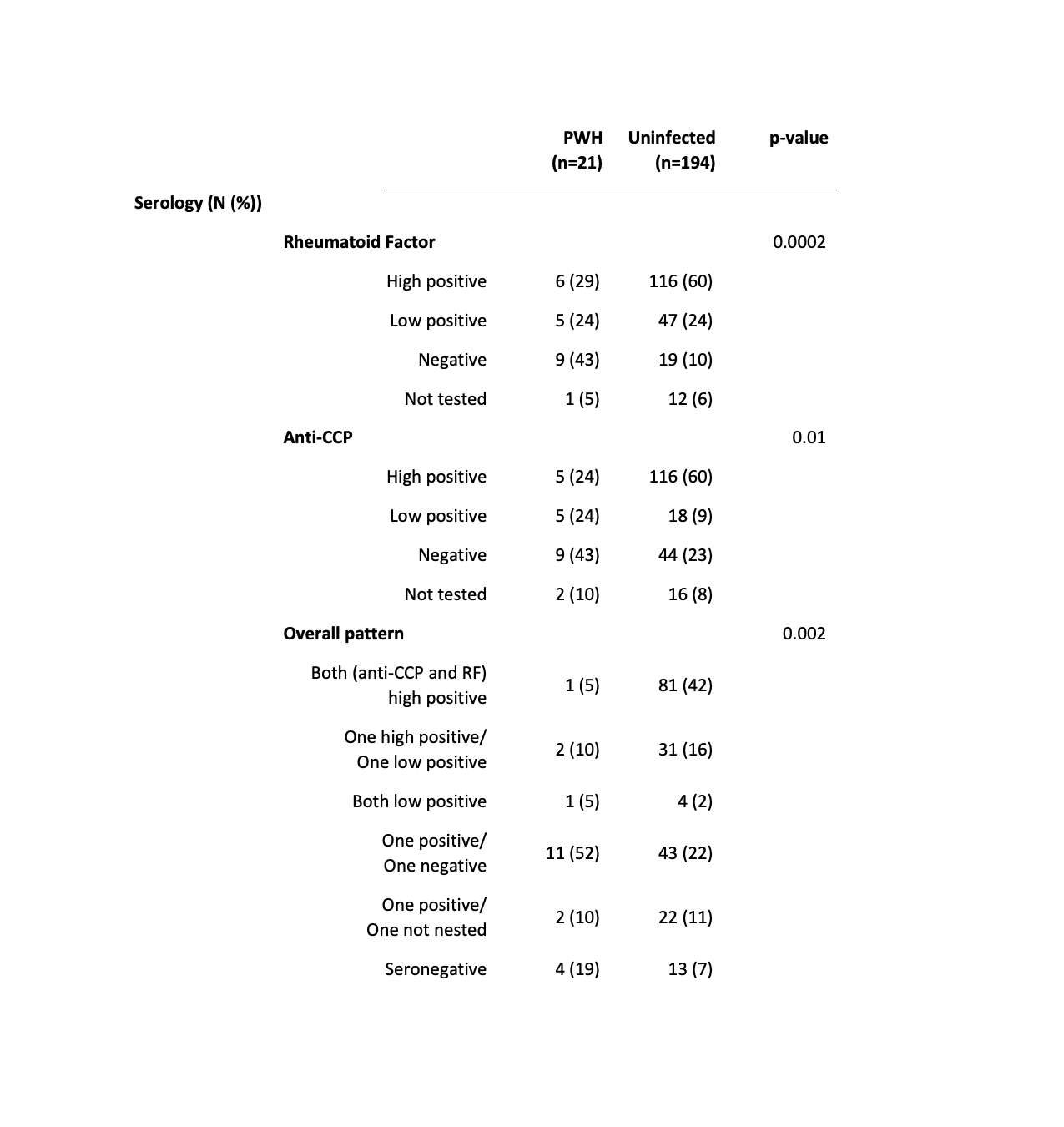 Table: Anti-CCP and Rheumatoid Factor Serologies Were More Strongly Positive in Uninfected than in PWH with Incident RA. High positive was defined in accordance with the 2010 RA Classification Criteria as at least 3 times the upper limit of normal per the local laboratory value. Low positive was defined as a result greater than the upper limit of normal but less than 3 times this value, or an unquantified positive result.
Table: Anti-CCP and Rheumatoid Factor Serologies Were More Strongly Positive in Uninfected than in PWH with Incident RA. High positive was defined in accordance with the 2010 RA Classification Criteria as at least 3 times the upper limit of normal per the local laboratory value. Low positive was defined as a result greater than the upper limit of normal but less than 3 times this value, or an unquantified positive result.
To cite this abstract in AMA style:
Hanberg J, Akgun K, Fraenkel L, Hsieh E, Justice A. Epidemiology and Characteristics of Incident Rheumatoid Arthritis in Persons with and Without HIV [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/epidemiology-and-characteristics-of-incident-rheumatoid-arthritis-in-persons-with-and-without-hiv/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-characteristics-of-incident-rheumatoid-arthritis-in-persons-with-and-without-hiv/
