Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
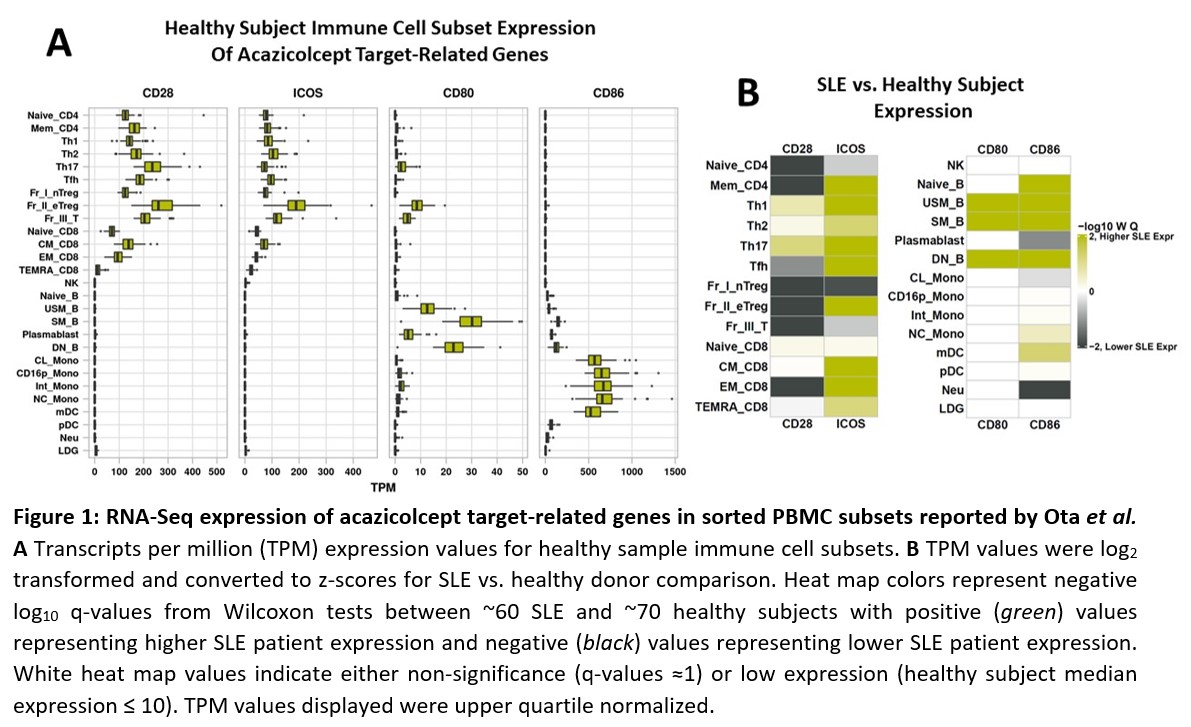
Background/Purpose: CD28 and inducible T cell costimulator (ICOS) play nonredundant roles in T cell activation and inhibiting these pathways can ameliorate an (auto)immune response. Systemic lupus erythematosus (SLE) is characterized by the dysregulation of T and B cell activation. Transcriptional analyses have revealed upregulation of CD28 and ICOS ligand/receptor genes in SLE1, but single pathway inhibition has not proven clinically effective in SLE and related diseases.2,3 Acazicolcept is an Fc fusion protein of a human variant ICOS-ligand (ICOSL) domain designed to block CD28 and ICOS simultaneously. We conducted in vitro assays with healthy donor (HD) and SLE patient PBMCs to analyze acazicolcept or comparators to suppress inflammatory mediators that promote disease pathogenesis. Additionally, acazicolcept was evaluated in a SLE mouse model.
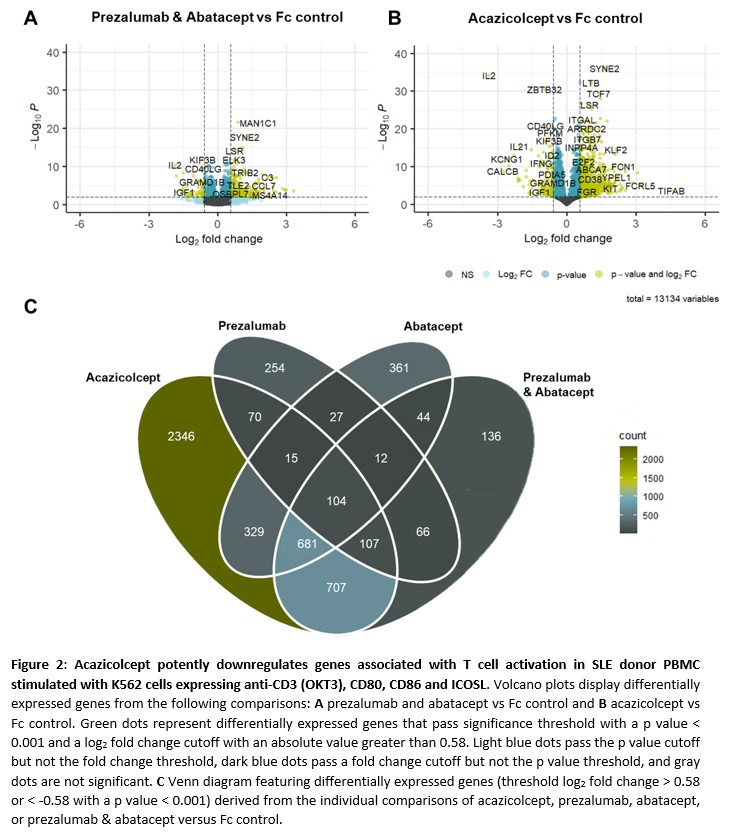
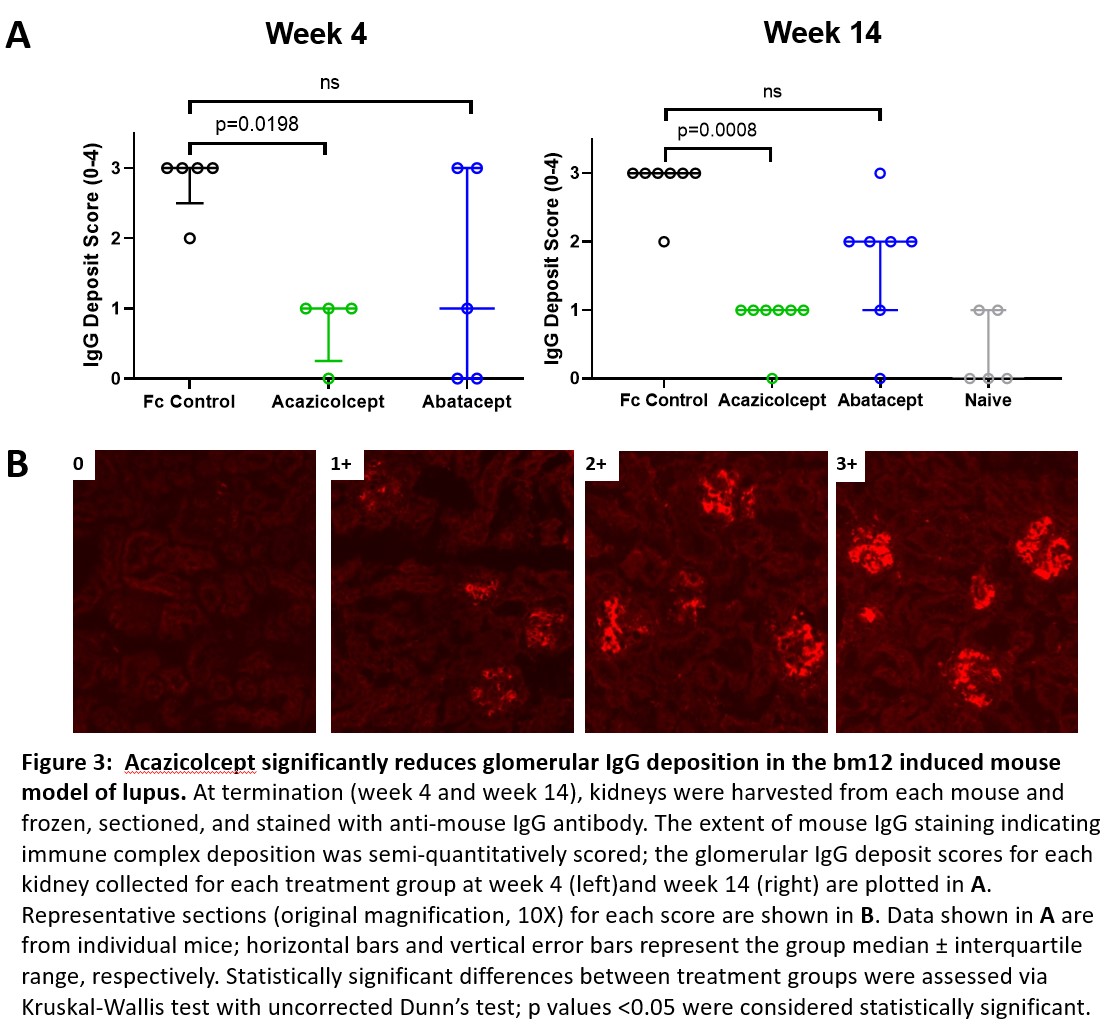
Methods: HD or SLE PBMCs were stimulated with artificial antigen presenting cells expressing CD80, CD86, ICOSL and anti-CD3 (OKT3) for 48h with 100 nM of Fc control protein, acazicolcept, or comparators directed against CD28 (abatacept, [CTLA-4-Ig]) or ICOS (prezalumab [anti-ICOSL mAb]) or combined abatacept/prezalumab. Supernatants and cells were analyzed for cytokine production and gene expression. Acazicolcept was compared in vivo to abatacept (CTLA4-Ig) in a bm12 induced mouse model of lupus4. C57BL/6 recipient mice were treated 2x/wk with acazicolcept or abatacept (N=12), from Days 0-93. Serum anti-double stranded (ds) DNA antibody concentrations were measured, and frozen kidney sections collected on Day 100 wereanalyzed for IgG deposition.
Results: Acazicolcept more potently suppressed expression of genes associated with T cell activation than the abatacept or prezalumab comparators, alone or combined. Gene expression analyses revealed distinct transcriptional profiles between PBMC from HD vs. SLE patients (Fig 1), in agreement with previously published findings. Furthermore, acazicolcept suppressed pro-inflammatory cytokine production and inhibited pathways associated with immune activation including Th1 and Th2 activation and IL-17 signaling (Fig 2). In the bm12 model, acazicolcept significantly reduced serum titers of anti-dsDNA autoantibodies compared to Fc control on Weeks 2 and 6. IgG deposition scores in the kidneys of acazicolcept-treated mice were significantly lower than the Fc control group at Weeks 4 (p=0.0198) and 14 (p=0.0008), while these scores in the abatacept-treated mice were not significantly different than the Fc control group (Fig 3).
Conclusion: Taken together, these and previous findings indicate that simultaneously inhibiting ICOS and CD28 pathways may result in significant disease amelioration in lupus-related inflammation/autoimmunity, with activity superior to agents targeting only one of these pathways. These observations provide further support for the clinical evaluation of acazicolcept for treatment of SLE; a Phase 2 trial of acazicolcept in SLE is ongoing (NCT04835441/Synergy).
1 Ota, M, et al. 2021. Cell. 184(11): 3006-21.
2 Cheng LE, et al. 2018. Arthritis Rheumatol. 70(7): 1071-6.
3 Pontarini, E, et al. 2020. Clin Exp Rheumatol. 38 Suppl 126(4): 222-7.
4 Klarquist, J., et al., 2015. J Vis Exp. (105): e53319.
To cite this abstract in AMA style:
Repash E, Blair T, Enstrom A, Evans L, Debrot S, Lewis K, Bankhead A, Peng S, Dillon S. Dual Blockade of ICOS and CD28 with Acazicolcept (ALPN-101) Reveals Non-Redundant Roles of T Cell Co-Stimulation Pathways in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/dual-blockade-of-icos-and-cd28-with-acazicolcept-alpn-101-reveals-non-redundant-roles-of-t-cell-co-stimulation-pathways-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/dual-blockade-of-icos-and-cd28-with-acazicolcept-alpn-101-reveals-non-redundant-roles-of-t-cell-co-stimulation-pathways-in-systemic-lupus-erythematosus/