Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Biological age (BA) may be superior to chronological age (CA) in predicting mortality and age-related conditions such as diabetes and cognitive/functional decline (PMID35715611), as well as osteoarthritis (OA). This study used measures of BA to estimate features of “accelerated aging” and associated these measures with multiple joint OA (MJOA) prevalence and pain.
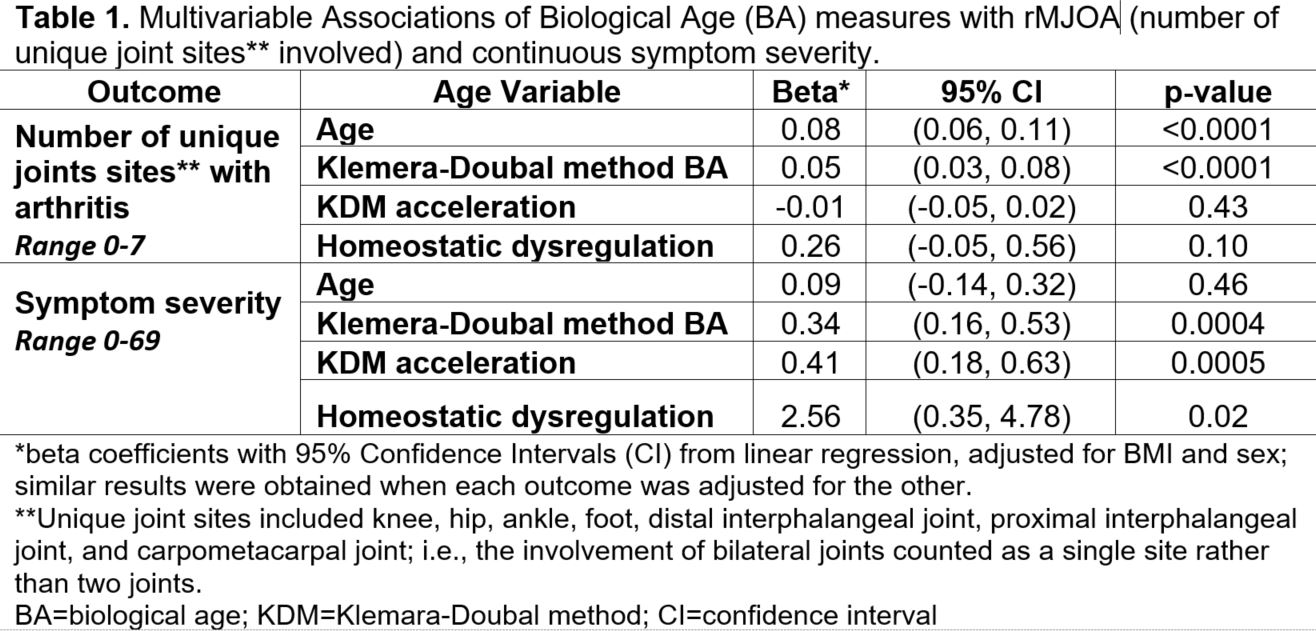
Methods: We used data from participants with and without OA enrolled in a substudy of the population-based Johnston County Health Study (JoCoHS) aiming to identify biomarkers predictive of MJOA development. Radiographic MJOA (rMJOA) was defined two ways: continuous number of unique joint sites involved (possible range 0-7, Table 1) and binary (presence = 3+ joint sites). Symptom severity was calculated as a sum of the pain/aching/stiffness scores at each joint (0-3, none-severe) using a map that included a graphical representation of 23 joints.
Six biomarkers collected routinely in clinical settings (i.e., albumin, alkaline phosphatase, hemoglobin A1c [HbA1c], gamma-glutamyl transpeptidase [GGT], and systolic/diastolic blood pressure) available in both the JoCoHS and the 3rd National Health and Nutrition Examination Survey (NHANES III, used to train our models), were analyzed. Klemera-Doubal method BA (KDM, PMID16318865) was calculated for each participant and age acceleration was calculated as the difference between BA and CA (i.e., KDM BA minus CA). Homeostatic dysregulation (HD, PMID23376244) was computed relative to a reference sample (i.e., non-pregnant, non-obese NHANES participants < 30 years). Regression models adjusted for sex and body mass index (BMI) were used to examine the association of KDM BA, HD, and CA with MJOA and symptom severity.
Results: One hundred JoCoHS participants (63% men, 33% Black, 13% Hispanic; mean age 56 ± 10 years (range 35-70), mean BMI 34 kg/m2) were included. One in 5 (21%) participants had rMJOA; mean number of painful joints was 8 (SD=6).
The mean KDM BA was 52 “years” (SD=11, range 28-82). The mean KDM acceleration was -4 (SD=9, range -23 to 22). Mean HD was 3.0 (SD=1.0, range 1-7, higher values represent greater deviation from reference). KDM was more closely correlated to chronological age (r=0.62) than was HD (r=0.15).
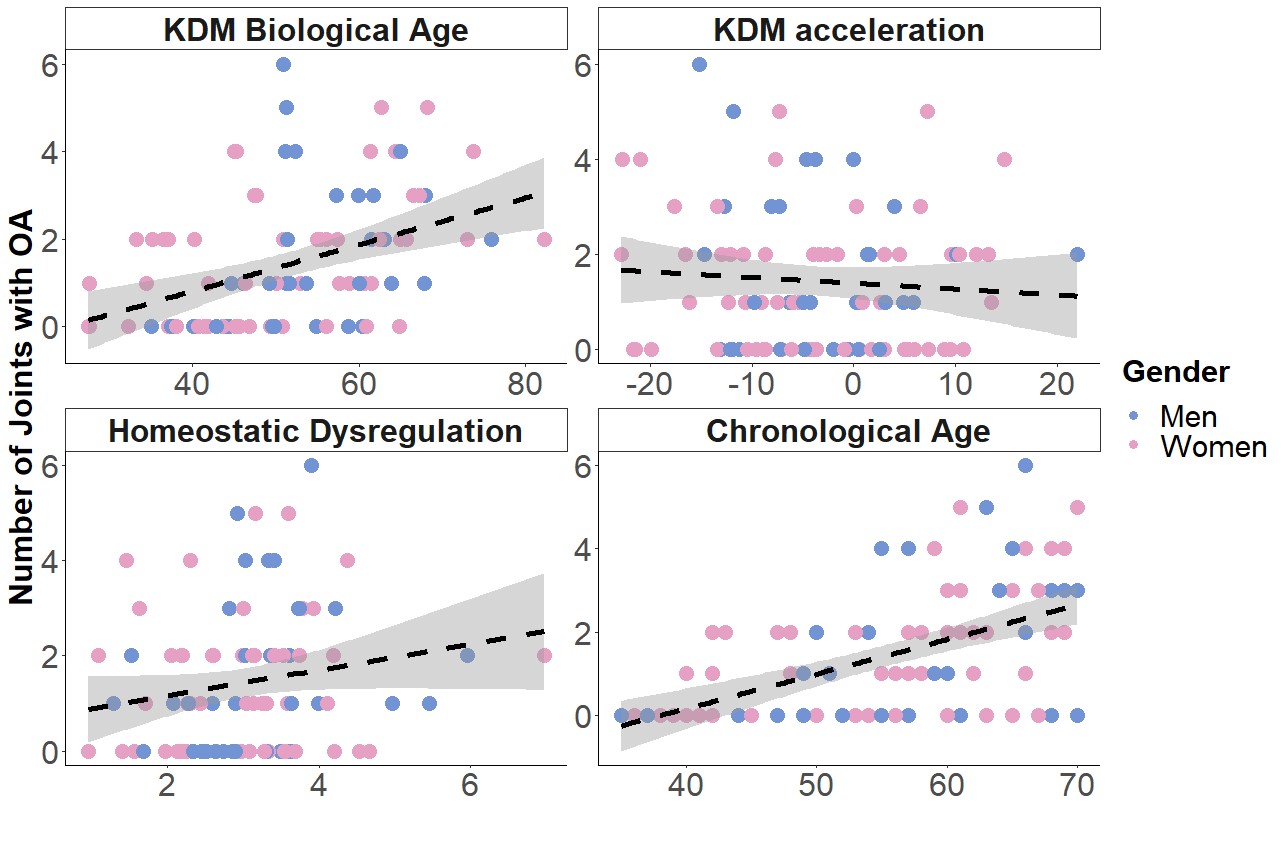
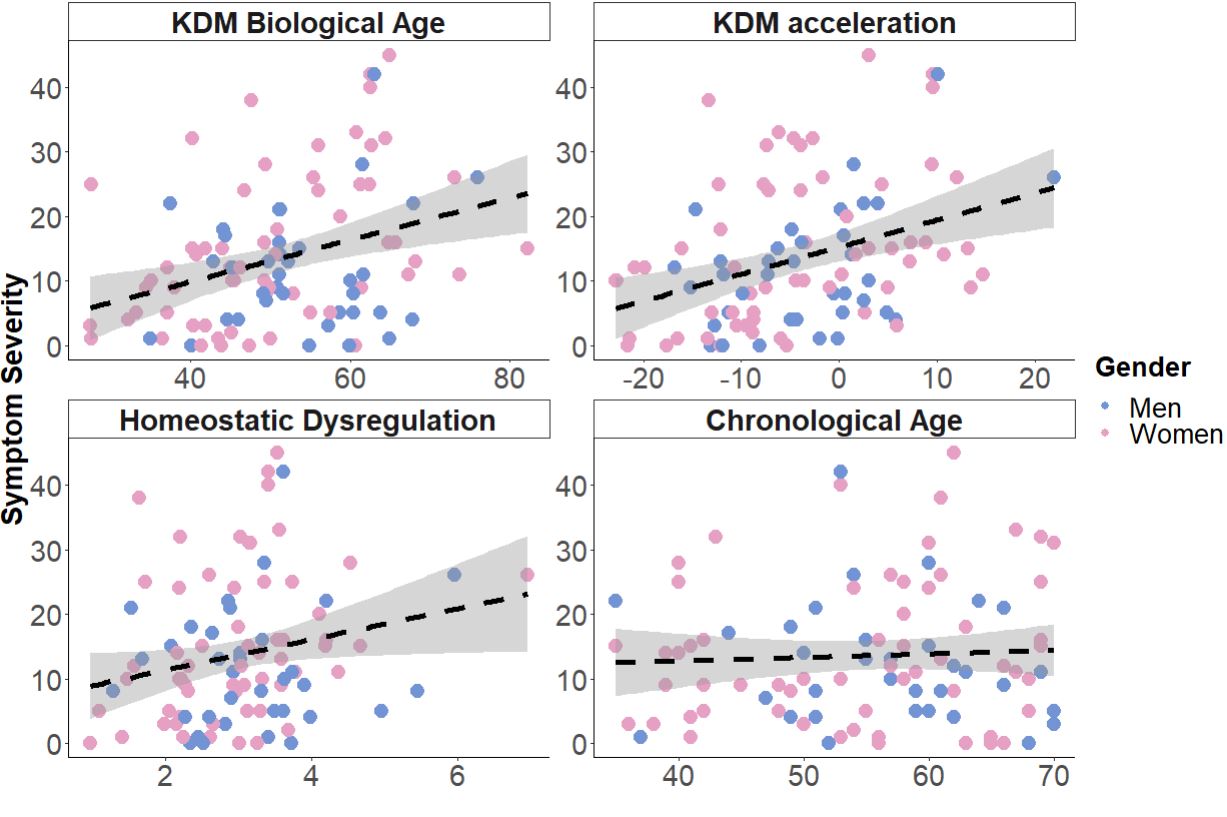
In the multivariate regression models (Table 1), CA and KDM BA were associated with rMJOA (CA: OR=3.8 per 5 years, 95% CI [2.1-7.8]; KDM BA: 1.4 [1.1-1.9]) and number of joint sites with OA, while age acceleration and HD were not associated with rMJOA. In contrast, while there was no association between CA and symptom severity, KDM BA, age acceleration, and HD were all statistically significantly associated with higher symptom severity. Scatterplots (Fig1 and Fig2) show unadjusted associations between age variables and the corresponding outcomes.
Conclusion: In regression models, CA was associated with rMJOA, but not with symptoms. BA measures were associated with increased symptom burden, while the association with rMJOA was less strong or not statistically significant. Our future work will add additional advanced biomarkers to this dataset to further understand the potential mechanisms underlying these associations.
To cite this abstract in AMA style:
Arbeeva L, Golightly Y, Kurz C, Jeffries M, Kraus V, Loeser R, Lascelles D, Nelson A. Discordant Associations Among Chronological and Biological Age with Multi-joint Osteoarthritis and Symptom Burden: The Johnston County Health Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/discordant-associations-among-chronological-and-biological-age-with-multi-joint-osteoarthritis-and-symptom-burden-the-johnston-county-health-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/discordant-associations-among-chronological-and-biological-age-with-multi-joint-osteoarthritis-and-symptom-burden-the-johnston-county-health-study/