Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Dermatomyositis (DM) is a rare autoimmune disease characterized by chronic muscle and skin inflammation. One potential complication of DM is calcinosis, the heterotopic calcification of soft tissue. The differences in depth and densities of these calcifications make early detection difficult by physical exam.Infrared imaging (IR) is a light-based modality that measures an object’s surface temperature. It has been used for other medical applications; however, IR imaging has not previously been employed for assessing DM-associated calcinosis. We proposed an IR algorithm to detect calcinosis in patients with juvenile and adult DM (J/DM) by measuring the value and variability of skin surface temperature. We believe its use will provide clinicians with a supplementary non-ionizing, inexpensive, and easy-to-use imaging modality to quantify DM-associated calcinosis at an early onset.
Methods: Study subjects were recruited from a myositis natural history study conducted at the National Institutes of Health in Bethesda, MD, and enrolled from August 2020 to July 2022. Inclusion criteria for the present study were probable or definite J/DM by Bohan and Peter criteria. Each patient also had suspicion of calcinosis, either self-reported or by documented assessment from a medical professional.Patient scans were conducted by an IR camera (ImageIR® 8300, InfraTec, Germany) at the NIH Clinical Center in Bethesda, MD. All scans were done in a temperature-controlled and humidity-monitored room (18-22 °C, 50-60 % humidity). Target scan locations were selected beforehand based on common calcinosis areas in J/DM, including the abdomen, back, arms, and legs. All images were taken as close to perpendicular to the patient as possible.
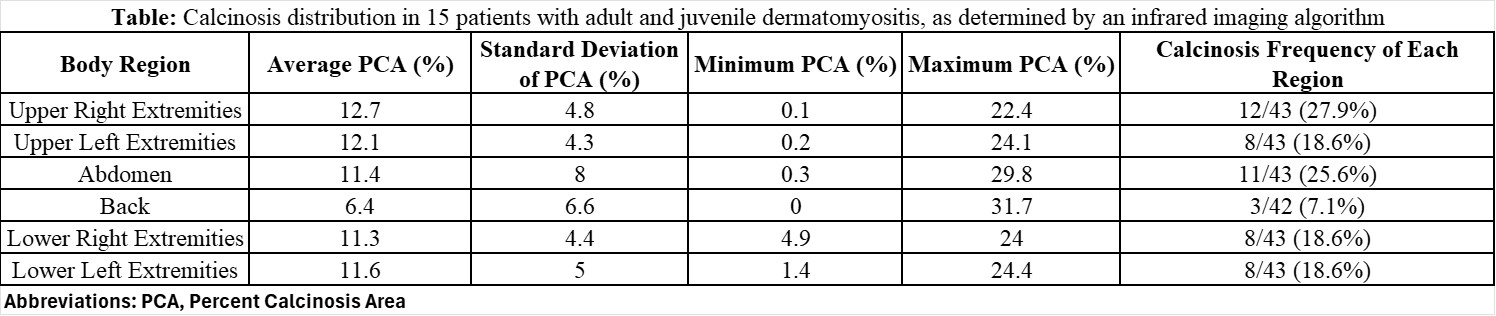
Results: Two hundred fifty-seven IR images from 3 DM and 12 JDM patients (age 9-60) were obtained from 6 body regions consisting of the right/left upper/lower extremities, abdomen, and back. For the population, the mean and range for CDASI activity, damage, and total calcinosis were (10, 2-41; 13, 2-25; 6, 2-11) respectively.The percent calcinosis area (PCA) was calculated as the pixels determined to contain calcinosis by the algorithm divided by the pixels determined to contain body area, multiplied by 100 to express the result as a percent. When PCA exceeded 15% to account for edge effect, the region was defined as positive for calcinosis. The calcinosis frequency of each region was calculated as the number of positive images of the region by its total number of images. The areas most and least frequently identified as positive for calcinosis by IR imaging were the upper right extremities and back, respectively.The IR algorithm’s suspected calcinosis areas ranged from 0.2% to 31.7%, with averages of each region ranging from 6.4 – 12.7% PCA (Table). Left and right extremities were within 0.6% of each other’s averages.Example IR image comparisons with traditional photography, physician exam, and CT are provided in Figure 1 and 2 from patients with calcinosis.
Conclusion: IR detected calcinosis in all body regions examined and demonstrated relative symmetry between left and right extremities. Further evaluation against other standards is required to validate the utility of IR in detecting calcinosis.
.jpg) Patient 1 had calcinosis in their left lower extremity distal to the knee. Image A is the IR image of this area and image B is the traditional photo of the same area. Image C is the physician drawing of the calcinosis from physical exam. Image D is the CT scan of the same area.
Patient 1 had calcinosis in their left lower extremity distal to the knee. Image A is the IR image of this area and image B is the traditional photo of the same area. Image C is the physician drawing of the calcinosis from physical exam. Image D is the CT scan of the same area.
Patient 2 had calcinosis in their right upper extremity proximal to the elbow. Image E is the IR image of this area and Image F is the traditional photo of the same area. Image G is the physician drawing of the calcinosis from physical exam. Image H is the CT scan of the same area.
To cite this abstract in AMA style:
Sachdeva S, Cervantes B, Rider L, Schiffenbauer A. Developing an Algorithm to Quantify Dermatomyositis-Associated Calcinosis Using Infrared Imaging [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/developing-an-algorithm-to-quantify-dermatomyositis-associated-calcinosis-using-infrared-imaging/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/developing-an-algorithm-to-quantify-dermatomyositis-associated-calcinosis-using-infrared-imaging/