Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Timely diagnosis of Juvenile Idiopathic Arthritis (JIA) enables early initiation of therapy, prevents accrual of joint damage, and improves outcomes. Data regarding the diagnostic process, including time to diagnosis, for patients in the United States is sparse. We aimed to evaluate the prevalence of and factors associated with 1) physical exam findings of longstanding disease at diagnosis and 2) longer time to diagnosis.
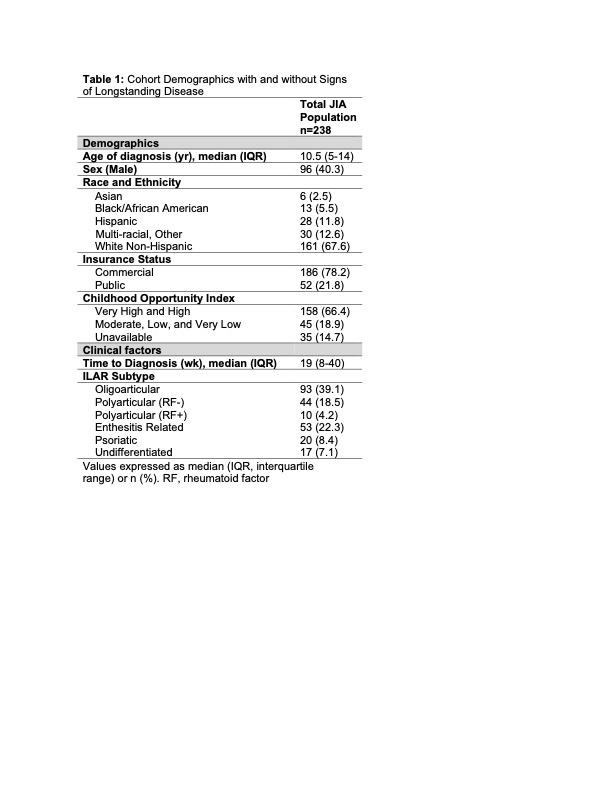
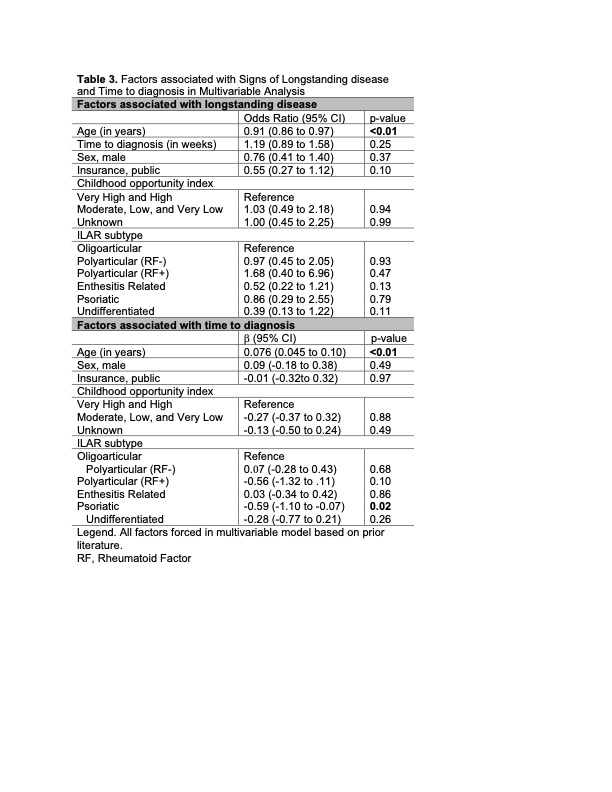
Methods: We performed a retrospective cohort study of patients with an incident JIA diagnosis at a tertiary academic center from January 2021 to December 2023. Patients were excluded if they had systemic JIA or Inflammatory Bowel Disease or were seen for a second opinion or transfer of care evaluation. Indicators of longstanding disease were chosen based upon published literature and included leg length discrepancy, muscle atrophy, contracture, micrognathia, and jaw asymmetry. Time to diagnosis was defined as time from reported symptom onset to date of diagnosis. Data was extracted from the electronic medical record. Differences amongst JIA subgroups were tested using chi-squared test for signs of longstanding disease (any vs none) and Kruskal-Wallis test for time to diagnosis. Factors associated with having at least 1 sign of longstanding disease at diagnosis were evaluated using logistic regression. Time to diagnosis was log-transformed to account for skewed distribution and association of risk factors with longer time to diagnosis was evaluated using linear regression.
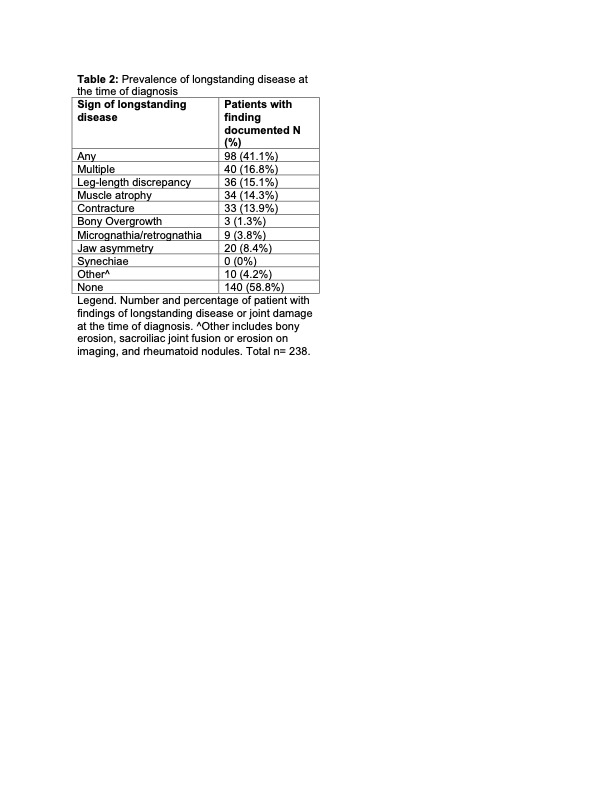
Results: 238 children were diagnosed with JIA during the study period (Table 1). 41.1% of patients had at least one sign of long-standing disease at diagnosis with leg-length discrepancy being the most common (15.1%; Table 2). 16.8% had ≥2 signs of longstanding disease. A higher proportion of patients with oligoarticular JIA had ≥1 indicator of longstanding disease (48%, p=0.02). In the multivariable logistic regression model younger age was the only factor associated with having ≥1 sign of longstanding disease (p=0.01). Interestingly, longer time to diagnosis was not significantly associated with presence of signs of longstanding disease. Median time to diagnosis was 19 weeks (IQR: 8 to 40, range: 1 to 311). Time to diagnosis was > 1 year in 23.5% of patients, and > 2 years in 11.7%. Median time to diagnosis amongst JIA subtypes was significantly different (p=0.01), with ERA patients having the most prolonged time (27 weeks). In the linear regression model, older age (p< 0.01) was associated with longer time to diagnosis and subtype of psoriatic arthritis (p=0.04) was associated with a shorter time to diagnosis (Table 3). The multivariable models for signs of longstanding disease and time to diagnosis could only explain 7% and 17%, respectively, of the variance.
Conclusion: It is common for patients with JIA to have signs of longstanding disease at the time of diagnosis. Even at a center with a minimal median wait time to next new patient visit, patients with JIA experience clinically significant delays in diagnosis. Multivariable regression models fail to explain a large proportion of the variance in the time to diagnosis or signs of longstanding disease suggesting there is much to learn about the drivers of diagnostic delay in JIA.
To cite this abstract in AMA style:
Costello A, Muir C, Xiao R, Weiss P, Rasooly I. Delayed Diagnosis and Accrual of Joint Damage in Incident Cases of Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/delayed-diagnosis-and-accrual-of-joint-damage-in-incident-cases-of-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/delayed-diagnosis-and-accrual-of-joint-damage-in-incident-cases-of-juvenile-idiopathic-arthritis/