Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Idiopathic Inflammatory Myopathies (IIM) are a group of rare systemic autoimmune conditions mainly characterized by muscle weakness, rash and involvement of various organs. Dermatomyositis (DM) and polymyositis (PM) are the major subtypes of IIM, although Necrotizing Myopathy and anti-Synthetase Syndrome are now considered distinct entities from PM. Corticosteroids are conventionally used as the first line treatment for patients with DM/PM; however, the risk of complications increases with long-term (LT) use of corticosteroids. This study evaluated the impact of LT oral corticosteroid (OCS) therapy on complications and use of existing treatments among patients with DM/PM.
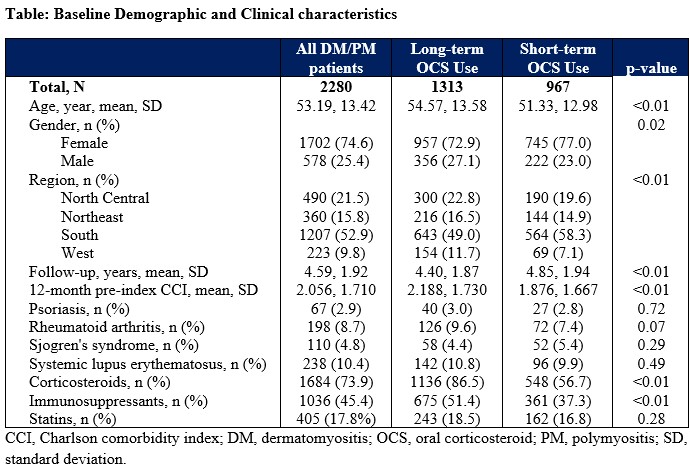
Methods: Adults who had ≥2 medical claims of DM/PM, with 30-365 days apart between 1/1/2016 and 12/31/2022 and ≥1 diagnosis code associated with physician specialty of interest (eg, rheumatologist), were selected from the IBM MarketScan® Commercial and Medicare Supplemental claims databases. Patients were required to have ≥1 pharmacy claims for OCS on or after the diagnosis date (date of the first OCS claim was designated as index date); ≥12 months pre-index and ≥12 months post-index continuous enrollment; and should not have a diagnosis of inclusion body myositis during the study period. Patients were classified into the LT group if they had continuous OCS use for ≥3 consecutive months (ie, no gaps >90 days from the dispensing date of previous prescription to the date of the next prescription or the end of data availability) within the 12-month post-index period, regardless of dosage; otherwise, they were classified into the short-term (ST) group. Multivariable logistic regressions were performed to evaluate the association of LT OCS use with presence of complications and use of advanced treatments after adjusting for baseline characteristics.
Results: A total of 2280 patients (mean [±SD] age: 53 [±13.4] years; female: 74.6%) were included, of which 1313 (57.6%) were in LT and 967 (42.4%) in ST group (Table). Compared with ST OCS users, LT OCS users had significantly higher incidence of heart failure (aOR, 1.83; 95% CI, 1.27-2.65), deep venous thrombosis (aOR, 1.88; 95% CI, 1.19-2.97), osteoporosis (aOR, 1.93; 95% CI, 1.41-2.64) and Cushing syndrome (aOR, 9.31, 95% CI, 1.22-71.09) after adjusting for baseline demographic (eg, age, sex) and clinical (eg, comorbid conditions) characteristics. The LT OCS group was more likely to use rituximab (aOR, 1.93; 95% CI, 1.40-2.65) or immunoglobulin (aOR, 2.07; 95% CI, 1.60-2.68) than the ST group during the post-index period, after adjusting for demographic and clinical characteristics.
Conclusion: LT OCS use in DM/PM leads to higher rates of complications and advanced treatment use. Findings highlight the limitations of OCS and further support unmet need among these patients. Disease management with novel treatments with advantageous safety profile utilized in the disease course may be clinically impactful.
To cite this abstract in AMA style:
Aggarwal R, Cai Q, Labson D, Crivera C, Zazzetti F. Complications and Treatment Use Associated with Long-term Oral Corticosteroid Therapy Among Patients with Dermatomyositis or Polymyositis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/complications-and-treatment-use-associated-with-long-term-oral-corticosteroid-therapy-among-patients-with-dermatomyositis-or-polymyositis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/complications-and-treatment-use-associated-with-long-term-oral-corticosteroid-therapy-among-patients-with-dermatomyositis-or-polymyositis/