Session Information
Date: Sunday, November 12, 2023
Title: (0252–0282) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Anti-ribonucleoprotein (RNP) and anti-Sm/RNP common motif antibodies play a critical role in diagnosing patients with systemic lupus erythematosus (SLE), mixed connective tissue disease (MCTD) or other connective tissue disease. Despite some common features between RNP and Sm/RNP antigens, such as sharing a 14-kd-reactive protein, they also carry significant structural differences. Anti-Sm antibodies frequently target B/B’, D1 and D3 proteins, whereas anti-RNP antibodies are directed towards 70-kd, A, C proteins. It is already well known that anti-RNP antibodies when presenting alone in patients with MCTD are closely related with Raynaud’s phenomenon and relatively rare renal involvement. Rheumatologists encounter patients with positive anti-Sm/RNP common motif antibodies with or without anti-RNP antibodies in different clinical scenarios. However, the clinical phenotype of patients presenting solely with anti-Sm/RNP antibodies, or in association with anti-RNP antibodies remains unknown.
Methods: We obtained approval from the Institutional Review Board at the University of Iowa Hospitals and Clinics and conducted a retrospective cohort study of patients, who tested positive for anti-RNP, and/or anti-Sm/RNP antibodies. The antibody profile was analyzed at the time of diagnosis. All patients were followed up by rheumatology clinic.
All data were retrieved from the existing medical records available through the EPIC database. Data analysis included demographic characteristics, clinical manifestations, organ involvement, disease duration, antibody titers.
Continuous variables were expressed as means ± standard deviation (SD) or median with minimum and maximum range, categorical variables as counts and percentages. Differences between groups were evaluated with the student’s t test or Mann-Whitney U test for continuous variables and Chi-square or Fisher’s exact test for categorical variables.
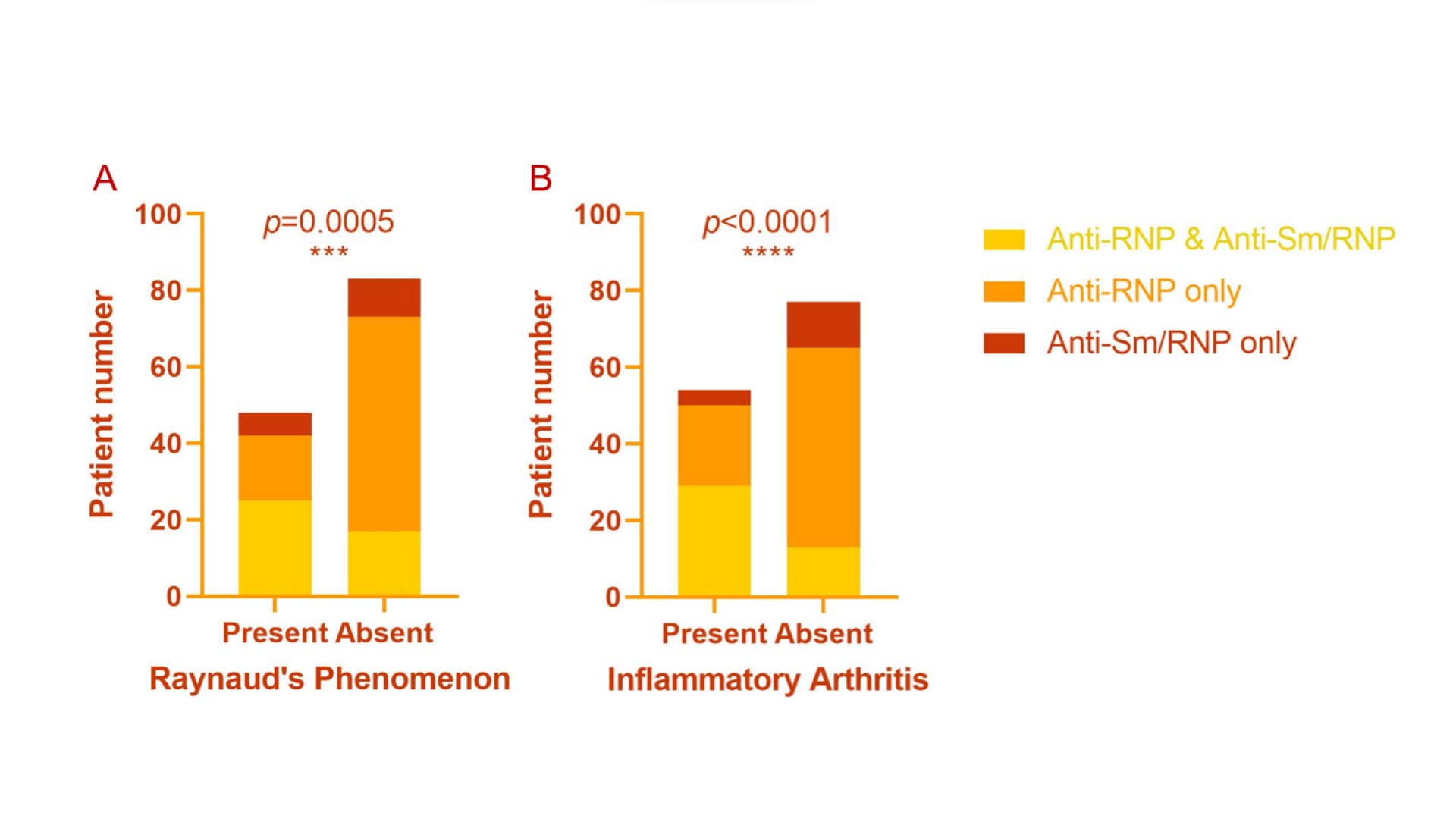
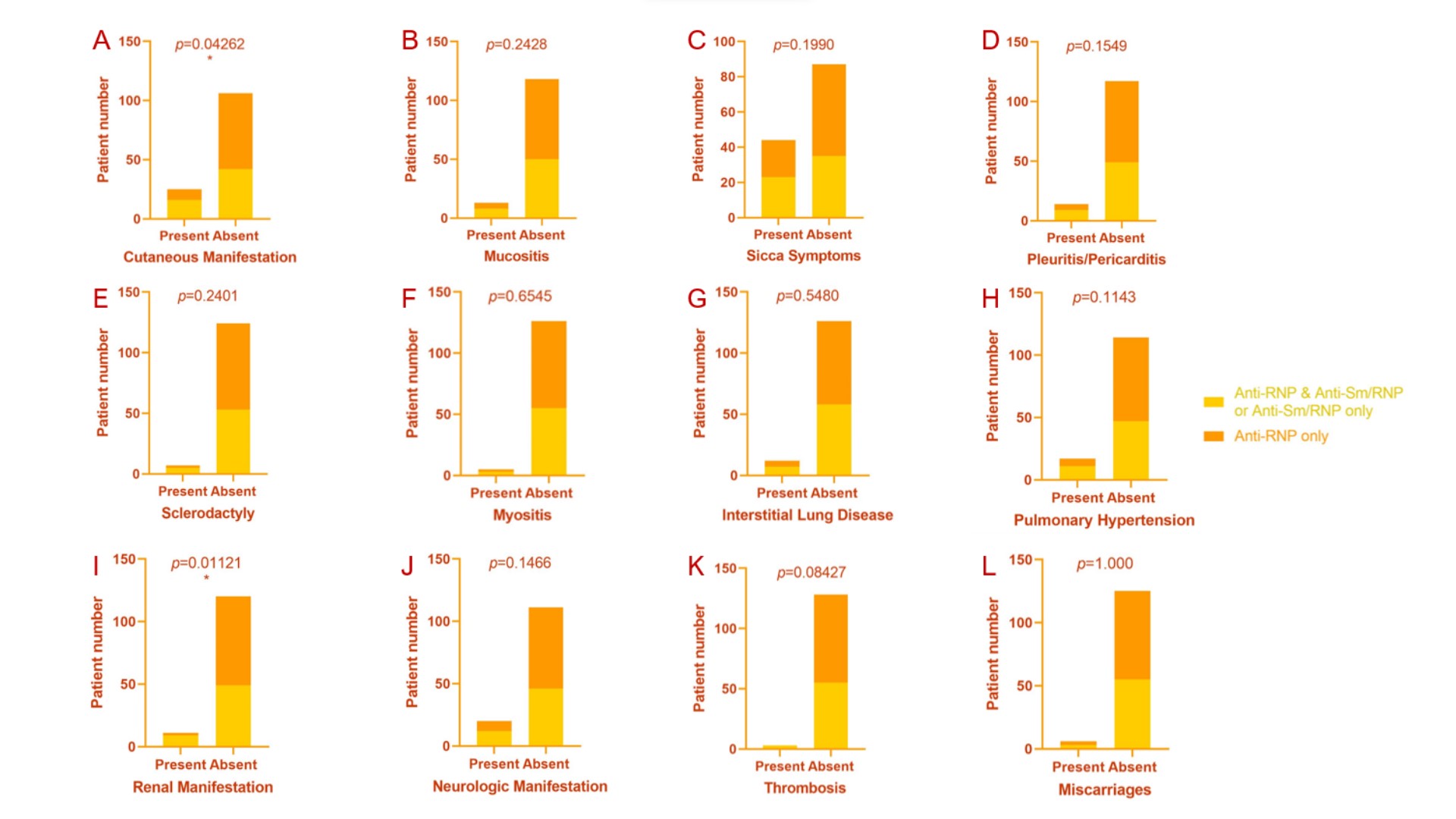
Results: A total of 131 patients were included in the study, of which 42 (32.1%) were tested positive for anti-RNP and anti-Sm/RNP antibodies, 73 (55.7%) positive for anti-RNP antibody only, 16 (12.2%) positive for anti-Sm/RNP only. 91.6% of patients were female and average age at diagnosis at our institute were 45 years old. The rate of inflammatory arthritis was significantly higher in patients positive for anti-RNP and anti-Sm/RNP antibodies than anti-RNP only or anti-Sm/RNP only (69.1% vs. 28.8% vs. 25.0%, p< 0.0001), as well as Raynaud’s phenomenon (59.5% vs. 23.3% vs. 37.5%, p=0.0005). Rash and renal manifestations were significantly more frequent in patients tested positive for anti-Sm/RNP with or without anti-RNP when compared with patients only positive for anti-RNP antibody. There was no significant difference in mucositis, sicca symptoms, pleuritis/pericarditis, sclerodactyly, myositis, interstitial lung disease, pulmonary hypertension, neurologic manifestations, thrombosis, or miscarriages.
Conclusion: The presence of anti-Sm/RNP common motif antibodies was more commonly associated with inflammatory arthritis, Raynaud’s phenomenon, and could be associated with rash and renal involvement.
To cite this abstract in AMA style:
Ni R, Lenert P. Clinical Phenotypes in Patients with Isolated Anti-Sm/RNP Common Motif Antibody Positivity, Compared to Those with or Without Associated Anti-RNP Antibody Reactivity [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/clinical-phenotypes-in-patients-with-isolated-anti-sm-rnp-common-motif-antibody-positivity-compared-to-those-with-or-without-associated-anti-rnp-antibody-reactivity/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-phenotypes-in-patients-with-isolated-anti-sm-rnp-common-motif-antibody-positivity-compared-to-those-with-or-without-associated-anti-rnp-antibody-reactivity/