Session Information
Date: Sunday, November 13, 2022
Title: Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Juvenile systemic sclerosis (jSSc) is a systemic fibroinflammatory autoimmune disease characterized by skin fibrosis and multiple extracutaneous manifestations. A proportion of children with jSSc have overlap disease, exhibiting features of other autoimmune diseases. There are no universally accepted classification criteria for this subset of patients. Though data is limited, recent adult and pediatric studies suggest that overlap disease represents a distinct clinical entity. This study evaluates the baseline clinical and serologic characteristics of patients with juvenile systemic sclerosis with overlap disease as compared to those without overlap features.
Methods: A cross-sectional study was performed using baseline visit data from patients enrolled in the National Registry for Childhood Onset Scleroderma (IRB PRO11060222), a prospective clinical and research registry of patients with juvenile-onset scleroderma evaluated at a single tertiary care institution with an associated multidisciplinary jSSc clinic. All patients fulfilled the 2013 ACR/EULAR criteria for SSc. Demographic, serologic, clinical, and laboratory data of interest were extracted. A comparison between jSSc with overlap disease and those without overlap features was performed using chi-square and Mann-Whitney U tests (significance defined a p < 0.05).
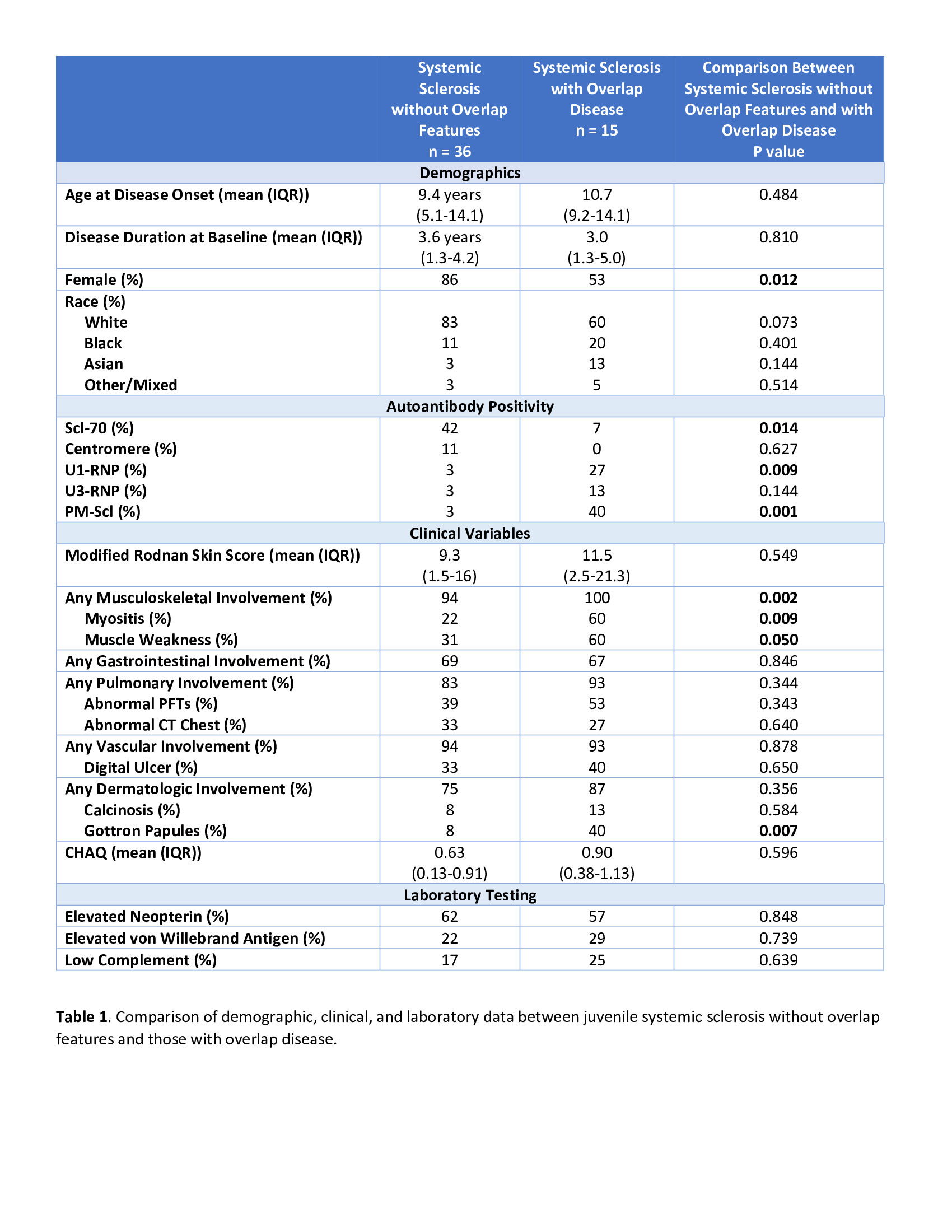
Results: Data for a total of 51 patients with jSSc were extracted. Of the jSSc patients that did not have overlap features (n = 36 (71%)), 64% had diffuse cutaneous, 14% had limited cutaneous, and 22% had unclassified subtypes. Overlap disease was relatively common (n = 15 (29%)). Of those with overlap disease, myopathic features were common (Table 1). One overlap disease patient had SLE and 2 patients had psoriatic arthritis. Patients with overlap disease were more likely to be male (47%) and have any musculoskeletal involvement (100%), myositis (60%), weakness (60%), and Gottron papules (40%) (p < 0.05). Autoantibody prevalence was significantly different between groups. Patients with overlap disease were more likely to be U1-RNP or PM-Scl antibody positive (27% and 40% respectively), while patients without overlap features were more likely to be Scl-70 positive (p < 0.05). Age at disease onset, age at baseline visit, race, modified Rodnan skin score (mRSS), prevalence of other organ system involvement, and laboratory studies of interest were otherwise similar between groups (Table 1).
Conclusion: Results from a single center jSSc cohort demonstrate significant differences between patients with overlap disease and those without overlap features. Similar to previous studies, overlap disease was common, was associated with more frequent musculoskeletal involvement, and had a unique autoantibody distribution. Interestingly, those with overlap disease were also more likely to be male. Additional clinical and translational studies are needed to further characterize this unique subset of patients. Improved clinical and immunologic characterization of these patients will allow for diminished diagnostic delay, focused evaluation and organ surveillance, and targeted therapeutics.
To cite this abstract in AMA style:
Robinson A, Torok K. Clinical and Serologic Characterization of Juvenile Systemic Sclerosis Overlap Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/clinical-and-serologic-characterization-of-juvenile-systemic-sclerosis-overlap-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-serologic-characterization-of-juvenile-systemic-sclerosis-overlap-disease/