Session Information
Date: Saturday, November 16, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Aminoacyl transfer RNA synthetase antibodies (ASAbs) are associated with a range of clinical manifestations, including severe lung and muscle disease and are postulated to be pathogenic. Published descriptions of the clinical associations and implications of antibody positivity are limited and have generally been drawn from specific diagnostic groups.
We describe the spectrum of clinical manifestations associated with ASAb positivity in an unselected population of patients from a single centre.To describe the spectrum of clinical manifestations associated with ASAb positivity in an unselected population of patients from a single centre.
Methods: The medical records of all patients recorded by the Hunter New England (HNE) pathology service with a positive ASAb between 2004 and 2023 were reviewed. Demographic details, indications for testing, specific ASAb findings, clinical manifestations, associations, and treatments were recorded through a search of HNE electronic records and direct contact with the treating physicians. A standard computer flatbed scanner with Euroimmun’s Euroline scanning software determined the intensity of staining. Descriptive statistics included frequencies for categorical variables and means with standard deviations for continuous variables. Frequencies were compared using Fisher’s exact test and means compared using a t-test. Analyses were performed with R v4.0.
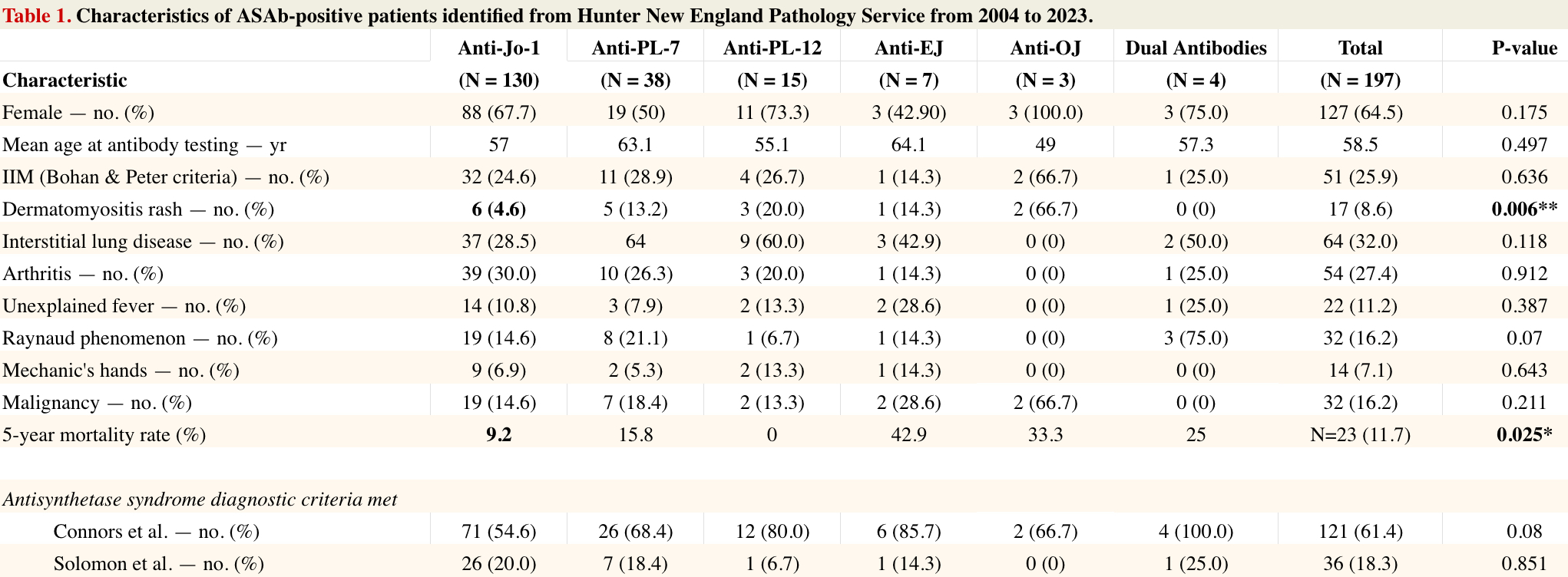
Results: 1440 patients tested for a myositis antibody. 1068 were excluded due to the absence of ASAb; 175 excluded for duplicate data or insufficient clinical information. 197 patients were included in the study
Interstitial lung disease (ILD) was present in 32% of patients, with a statistically higher rate in anti-PL-12 patients (60%, p=0.024) compared to other ASAb patients. An NSIP radiological pattern was statistically more frequent in the anti-Jo1 group (p=0.002).
Myositis was present in 25.9%. A specific perimysial/perifascicular myopathic histological pattern was exclusive to anti-Jo-1 patients. Dermatomyositis skin findings were statistically less common in anti-Jo-1 patients (4.6%, p=0.008). Five-year mortality was lowest in anti-Jo-1 and anti-PL-12 patients (p=0.025). There was no increased risk of malignancy. Mechanic’s hands were seen in 7.1% of patients, arthritis in 27.4%, unexplained fever in 11.2%, weight loss in 16.8%, and fatigue in 40.1%. Diagnostic criteria were met in 61.4% of cases using Connors’ criteria and in 18.3% using Solomon’s criteria
Conclusion: This is the largest single centre study of ASAbs to date in a general population of patients, uniquely unbiased by using the antibody as a starting point rather than specific diagnostic groups the finding of a positive antibody was associated with a variety of clinical phenotypes. While no specific association was identified with particular antibody subtypes there was indication that ILD may be increased in the anti-PL12 group and a perimysial/perifascicular muscle biopsy pattern was exclusively found in the Anti-Jo-1 group.
A borderline/weak positive antibody result can be linked to clinically significant disease.
The study provides a platform to further explore pathogenicity and the clinical implications of ASAbs
To cite this abstract in AMA style:
Kasto D, McLucas M, Aubin A, Faigl A, Major G. Characteristics of Patients with Antisynthetase Antibodies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-patients-with-antisynthetase-antibodies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-patients-with-antisynthetase-antibodies/