Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjögren’s disease (SjD) is a systemic disorder characterized by exocrine gland inflammation, leading to dry eyes/mouth, and multiple organ systems involvement1. The European League Against Rheumatism (EULAR) developed the Sjögren’s Syndrome Disease Activity Index (ESSDAI) to capture systemic disease activity across clinical domains, to monitor disease progression and guide treatment2.Patients with SjD often have comorbidities across multiple ESSDAI domains – musculoskeletal, central nervous system (CNS), hematological, pulmonary, renal, and others – significantly affecting morbidity, quality of life, and clinical management strategy 3.This study evaluates the prevalence of ESSDAI domain-specific comorbidities and treatment in patients diagnosed with SjD as well as those without any overlapping autoimmune conditions (2019–2023).
Methods: A retrospective cohort study using Optum Clinformatics® Data Mart (2019–2023) included adults (≥18 years) with ≥1 inpatient or ≥2 outpatient SjD claims. All relevant domain-specific comorbidities were identified using ≥2 ICD-10-CM diagnosis codes/year. Treatments assessed included biologics, immunosuppressants, NSAIDs, opioids, and neuropathic agents. Descriptive analyses were conducted for overall SjD patients and SjD patients without overlapping autoimmune disease, by calendar year.
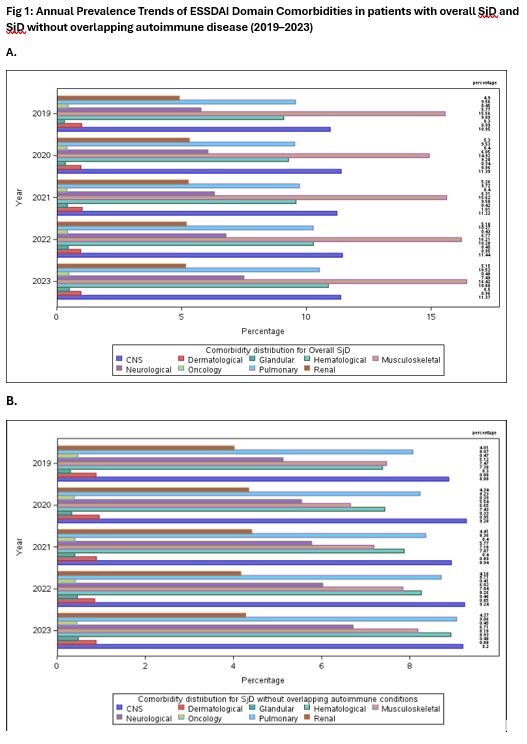
Results: In the overall SjD patients (n=38,456) and SjD patients without overlapping autoimmune conditions (n=24,657), majority were female (90.6%, 89.3%), most were aged ≥65 years (62.8%, 66.2%), and predominantly identified as non-Hispanic (77.6%, 78.9%) and White (68.1%, 69.6%), followed by Black (10.3%, 9.3%) and Asian (2.6%, 2.7%).In the overall SjD cohort, musculoskeletal comorbidities were the most prevalent (15.66-16.42%) while CNS involvement was highest in those without overlapping autoimmune conditions (8.88-9.20%). Both cohorts showed consistently high rates of hematological, pulmonary, and neurological domains. In both cohorts, fibromyalgia was the most prevalent CNS condition (~8–10%), hypokalemia was the leading renal comorbidity (up to 4.34%), and anemia was highest among hematological conditions (7.80–9.28%).SjD patients without overlapping autoimmune conditions had lower comorbidity prevalence versus overall SjD cohort (Table 1). Top treatments for both cohorts included hydroxychloroquine (32.8% vs. 28%), cyclosporine (~12%), azathioprine, rituximab, and adalimumab (Figure 2). The overall SjD patient cohort had consistently higher treatment rates.
Conclusion: Musculoskeletal, CNS, hematologic, pulmonary and neurological domains contribute substantially to high comorbidity burden in overall SjD patients and those without overlapping autoimmune conditions. High comorbidity and treatment rates were seen in both overall SjD and SjD without overlapping autoimmune conditions suggest a more complex disease phenotype, underscoring the need for targeted treatment strategies.References1. Mariette, X, et al. (2018). N Engl J Med, 378(10), 931-939.2. Seror, R, et al. (2015). Ann Rheum Dis, 74(5), 859-866.3. Brito-Zerón, P, et al. (2016). Nat Rev Dis Primers, 2(1), 16047.
To cite this abstract in AMA style:
Ganguli M, Kilby A, Shahabi A, Jay Lin T. Burden of Comorbidities Across EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) Domains: Treatment Prevalence Among Commercially Insured Sjögren’s Patients in the United States [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/burden-of-comorbidities-across-eular-sjogrens-syndrome-disease-activity-index-essdai-domains-treatment-prevalence-among-commercially-insured-sjogrens-patients-in-the-united-states/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/burden-of-comorbidities-across-eular-sjogrens-syndrome-disease-activity-index-essdai-domains-treatment-prevalence-among-commercially-insured-sjogrens-patients-in-the-united-states/

.jpg)
.jpg)