Session Information
Session Type: Abstract Session
Session Time: 11:00AM-11:50AM
Background/Purpose: Activation of the alternative and common terminal complement pathways has been shown in ANCA-associated vasculitis (AAV). Circulating titers of the anaphylatoxin C5a are increased and correlate with disease activity in AAV. Binding to the corresponding G protein-coupled receptor (C5aR1/CD88) enhances the influx of neutrophils and their activation, leading to ROS generation and endothelial damage. Blocking of the receptor C5aR1 was protective in a murine model of NCGN in AAV (4). In humans, the oral C5aR1 inhibitor avacopan showed promising results as glucocorticoid-sparing agent in two randomized phase 2 trials. The phase 3 trial was reported to have met its primary endpoints (NCT02994927). Notably, disease-specific anti-G protein-coupled receptor autoantibody (aab) signatures have been found in different autoimmune diseases, but have not been evaluated in AAV so far.
The aim of the present study was to examine whether circulating anti-C3aR and anti-C5aR1 autoantibodies (aabs) correlate with clinical findings in AAV and are linked to the clinical outcome. Values of anti-C3aR and anti-C5aR1 aabs AAV were analyzed and correlated with the clinical course.
Methods: Sera and plasma of AAV patients [granulomatosis with polyangiitis (GPA), n=64; microscopic polyangiitis (MPA), n=26; eosinophilic granulomatosis with polyangiitis (EGPA), n=11] were measured in a cross-sectional analysis by enzyme-linked immunosorbent assay (ELISA) for circulating autoantibodies against anti-C3aR and anti-C5aR1 aabs and plasma levels of C3a and C5a. Expression of C3aR and C5aR1 on T-cells and neutrophils was determined using flow cytometry. Clinical data including Birmingham vasculitis activity score (BVAS V3.0) were assessed at the time of serum sampling and during follow-up for 48 months.
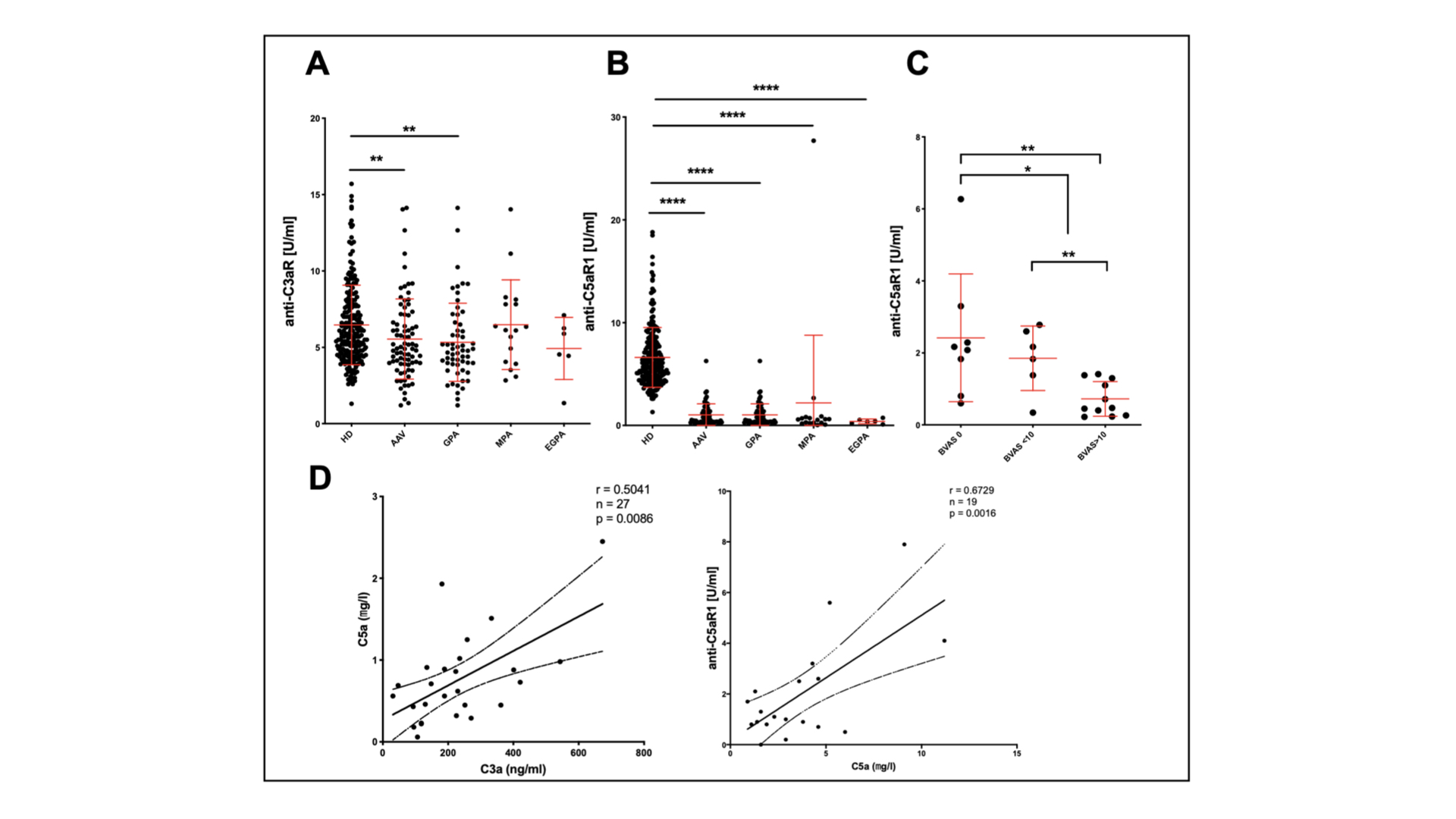
Results: Patients with GPA displayed low titers of anti-C3aR aabs (Fig. 1a, p≤0.05). Anti-C5aR1 aabs were decreased in AAV, especially in GPA (Fig.1b, p≤0.0001). GPA patients with a high BVAS had the lowest levels of anti-C5aR1 aabs Fig. 1c, p≤0.01). Plasma levels of C3a and C5a correlated positively in GPA. C5a and anti-C5aR1 levels correlated positively in GPA (Fig.1d). C5aR1 expression was increased on T-cells in GPA (Fig. 2). Titers of anti-C5aR1 aabs < 0.45U/ml correlated with an increased relapse risk for major relapse in GPA (Fig. 3; HR 12.85, P=0.0014).
Conclusion: Anti-C5aR1 aabs reflect complement activation and disease activity in GPA. Moreover, Anti-C5aR1 aabs may be useful to monitor disease activity. C5aR1 expression on T-cells may also play a role in AAV-pathogenesis.
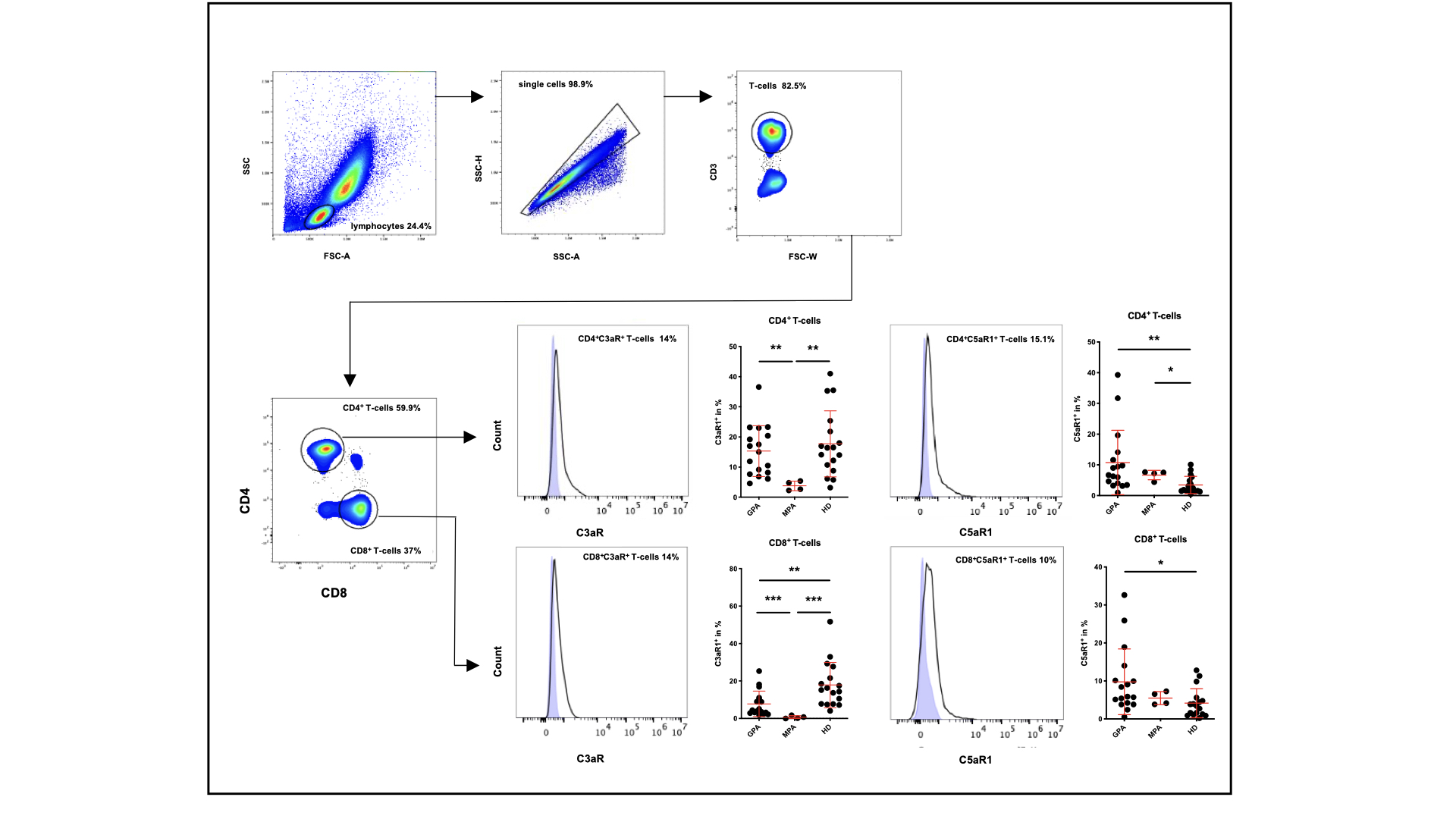 Figure 2 C5aR1 is overexpressed on CD4+ and CD8+ T-cells in GPA. Gating strategy of circulating CD4+ and CD8+ T-cells focused on the surface expression of C3aR and C5aR1 (Histogram: for comparison, shade blue area presented the isotype control). Data are presented as mean±SD; Mann-Whitney U-tests were used to determine significance *p≤0.05, **p≤0.01 and ***p≤0.001; HD, healthy donors; GPA, granulomatosis with polyangiitis; MPA, microscopic polyangiitis; FSC, forward scatter; SSC, side scatter
Figure 2 C5aR1 is overexpressed on CD4+ and CD8+ T-cells in GPA. Gating strategy of circulating CD4+ and CD8+ T-cells focused on the surface expression of C3aR and C5aR1 (Histogram: for comparison, shade blue area presented the isotype control). Data are presented as mean±SD; Mann-Whitney U-tests were used to determine significance *p≤0.05, **p≤0.01 and ***p≤0.001; HD, healthy donors; GPA, granulomatosis with polyangiitis; MPA, microscopic polyangiitis; FSC, forward scatter; SSC, side scatter
 Figure 3 Anti-C5aR1 aab levels below 0.45 U/I were associated with higher relapse rates in AAV, especially in GPA A: AAV patients with reduced titers of anti-C5aR1 aab < 0.45U/ml displayed an increased relapse risk, especially in GPA (B). C: Risk of major relapse for in AAV and GPA (D) (AAV: HR: 11.93, p < 0.0001; GPA: HR: 12.85, p=0.0014); AAV, ANCA-associated vasculitis; GPA, granulomatosis with polyangiitis
Figure 3 Anti-C5aR1 aab levels below 0.45 U/I were associated with higher relapse rates in AAV, especially in GPA A: AAV patients with reduced titers of anti-C5aR1 aab < 0.45U/ml displayed an increased relapse risk, especially in GPA (B). C: Risk of major relapse for in AAV and GPA (D) (AAV: HR: 11.93, p < 0.0001; GPA: HR: 12.85, p=0.0014); AAV, ANCA-associated vasculitis; GPA, granulomatosis with polyangiitis
To cite this abstract in AMA style:
Klapa S, Müller A, Koch A, Kerstein-Staehle A, Kaehler W, Heidecke H, Schinke S, Huber-Lang M, Nitschke M, Pitann S, Karsten C, Riemekasten G, Lamprecht P. Autoantibodies Targeting Complement Receptors C3aR and C5aR1 Are Decreased in ANCA-associated Vasculitis and Correlate with a Higher Relapse Rate [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/autoantibodies-targeting-complement-receptors-c3ar-and-c5ar1-are-decreased-in-anca-associated-vasculitis-and-correlate-with-a-higher-relapse-rate/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibodies-targeting-complement-receptors-c3ar-and-c5ar1-are-decreased-in-anca-associated-vasculitis-and-correlate-with-a-higher-relapse-rate/