Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The lung airways have been implicated in the pathogenesis of RA. RA-associated autoantibodies, including anti-cyclic citrullinated peptide (anti-CCP) antibodies are found to be generated in the lung using induced sputum. Epidemiologic studies have identified that the presence of airways diseases, such as asthma, increase incident RA compared to healthy cohorts. However, it remains unclear how this relationship between asthma and RAdevelops. The aim of our study was to investigate the relationship between asthma severity and serumanti-CCP in cross-section andover time.
Methods: Our prospective cohort study included patients with mild, moderate, and severe asthma. One-hundred forty-four patients were included in this study. Serum anti-CCP-IgG (CCP3, Werfen) and anti-CCP-IgA (research modification of CCP3.1, Werfen) levels were measured in by ELISA in banked serum obtained at baseline and at a longitudinal visit, which was separated by four years. Cut off levels for anti-CCP positivity was determined based on 3 standard deviations above the mean level in a separate cohort of 100 non-RA controls. Comparison between anti-CCP titers across asthma severity groups were carried out via t-test where appropriate. Each participant was determined to have mild, moderate or severe asthma at their baseline visit based on previously published expert guidelines (1).
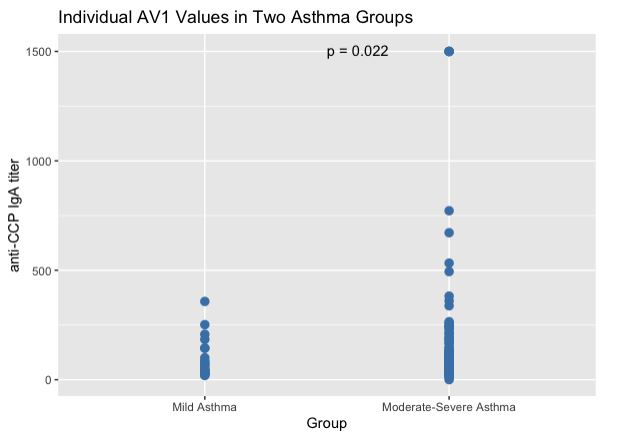
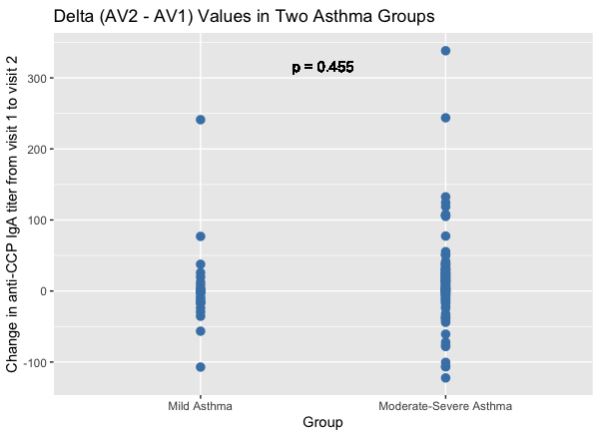
Results: Thirty-four of 144 (23.6%) were positive for anti-CCP-IgA and 2 were positive for anti-CCP-IgG (1.3%). Baseline serum anti-CCP-IgA levels were higher in patients with moderate or severe asthma compared to the mild asthma group (p=0.022, Figure 1), which remained significantly different at follow-up (p = 0.01).Both groups had an increase in mean anti-CCP-IgA levels at follow-up, although the moderate or severe group had a numerically higher increase that did not reach statistical significance (p = 0.46, Figure 2) There was no difference in serum anti-CCP-IgG levels based on asthma disease severity at baseline or follow-up (p = 0.69 and p = 0.18 respectively).
Conclusion: We found serumanti-CCP-IgA antibodies in a modest number of asthma patients. Interestingly, there was a significant association between asthma severity and anti-CCP-IgA level, suggesting a potential relationship between airways inflammation and development of anti-CCP antibodies in these individuals. Additionally, worse baseline asthma severity (mild vs moderate/severe) had a numerically higher anti-CCP increase which did not reach statistical significance but may support the role of airway disease severity in anti-CCP generation. There was no association with anti-CCP-IgG titers which supports the role of lung mucosa in the development of this relationship.
To cite this abstract in AMA style:
Rorah D, Ngo L, Castro M, Demoruelle K, Matson S. Asthma Severity Is Associated Increased Serum Anti-cyclic Antibody Level at Baseline and in Increase During Longitudinal Follow-up [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/asthma-severity-is-associated-increased-serum-anti-cyclic-antibody-level-at-baseline-and-in-increase-during-longitudinal-follow-up/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/asthma-severity-is-associated-increased-serum-anti-cyclic-antibody-level-at-baseline-and-in-increase-during-longitudinal-follow-up/