Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Infections are a major contributor to morbidity and mortality in patients (pts) with rheumatoid arthritis (RA). Little is known about the risk of non-serious infections, however, which are much more common than serious infections. This study aimed to use baseline data from an ongoing longitudinal study to identify factors associated with both serious infection in the past year and recent non-serious infection.
Methods: Pts with RA from a national rheumatology community practice-based research network, the Excellence Network in RheumatoloGY (ENRGY), were remotely recruited July 2022 to May 2023 to join a prospective 6-month study. Results of baseline surveys are reported, with longitudinal data collection ongoing. Interested pts were asked to join the ArthritisPower research registry to complete monthly assessments about their physical, mental, and social health, physical function, infections, and medication use. At baseline, pts reported recent antibiotic use in the preceding 3 months and hospitalization due to infection in the preceding year, as proxies for non-serious and serious infection, respectively. We hypothesized that older age, glucocorticoid use, DMARD type, comorbidities, and measures of more severe disease would be associated with greater frequency of both serious and non-serious infection.
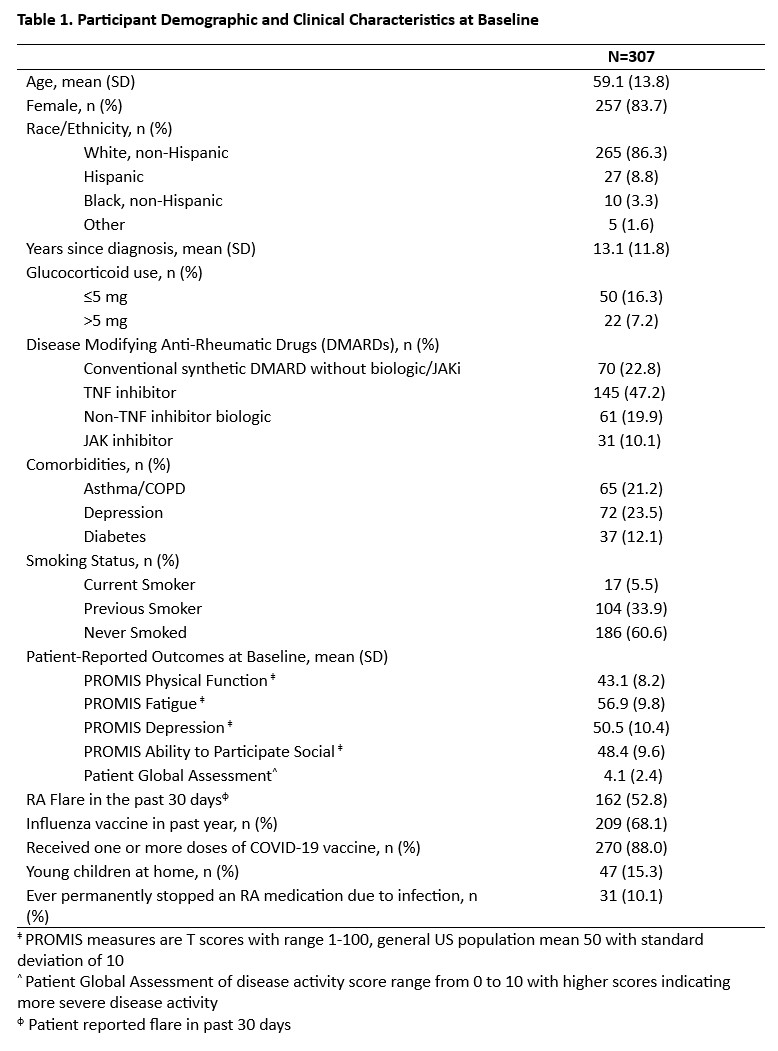
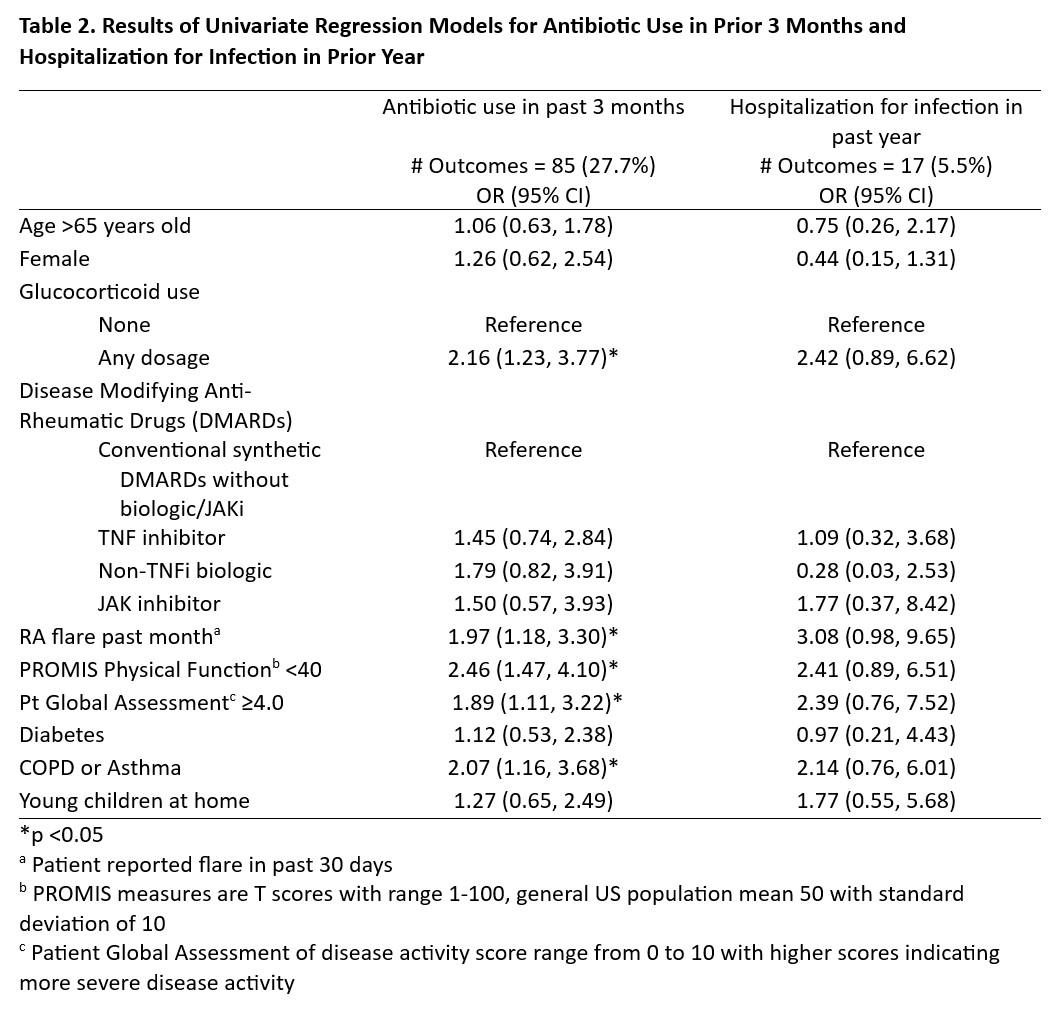
Results: At time of analysis, 307 pts with RA completed the baseline assessments. The mean (SD) age was 59 (14), 84% female, 86% non-Hispanic white (Table 1). TNF inhibitors were used by 47% of pts and 23% of pts were taking glucocorticoids, most commonly at doses ≤5 mg/day. Thirty-one pts (10%) reported permanently stopping RA medication in the past because of an infection. A total of 85 pts (28%) reported antibiotic use in the preceding 3 months and 17 (6%) reported hospitalization for infection in the preceding year (Table 2). Antibiotic use was associated with current glucocorticoids [OR 2.2 (95% CI, 1.2, 3.8)], recent RA disease flare [2.0 (1.2, 3.3)], worse PROMIS physical function < 40 [OR 2.5 (1.5, 4.1)], worse patient global ≥4 [1.9 (1.1, 3.2)], and asthma/COPD [OR 2.1 (1.2, 3.7)]. These factors were similarly associated with hospitalization although differences were not statistically significant (Table 2). Associations between DMARD type and both outcomes were modest and not statistically significant (Table 2).
Conclusion: Patients with RA with glucocorticoid use, recent disease flares, and poorer physical function and disease severity measures were more likely to report recent antibiotic use in the preceding 3 months and hospitalization in the past year. Both disease activity and treatment, particularly glucocorticoids, may affect both risk of serious infections and more common non-serious infections. Infections also influence treatment decisions, however, and pts not infrequently reported stopping medications because of infections. Accounting for disease activity and the potential that certain medications may be avoided in high risk patients (confounding by indication) are important when assessing infection risk with medications, and will be a focus of the longitudinal analysis from this cohort.
‡ PROMIS measures are T scores with range 1_100, general US population mean 50 with standard deviation of 10
^ Patient Global Assessment of disease activity score range from 0 to 10 with higher scores indicating more severe disease activity
φ Patient reported flare in past 30 days
*p <0.05
a Patient reported flare in past 30 days
b PROMIS measures are T scores with range 1_100, general US population mean 50 with standard deviation of 10
c Patient Global Assessment of disease activity score range from 0 to 10 with higher scores indicating more severe disease activity
To cite this abstract in AMA style:
Gavigan K, Rivera E, Kolenky O, Clinton C, Holladay E, Curtis D, Stradford L, Curtis J, Nowell W, Curtis C, George M. Association of Treatment and Disease Activity with Antibiotic Use and Hospitalized Infection Among People Living with Rheumatoid Arthritis: Baseline Data from a Longitudinal Study in the ArthritisPower Registry [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-of-treatment-and-disease-activity-with-antibiotic-use-and-hospitalized-infection-among-people-living-with-rheumatoid-arthritis-baseline-data-from-a-longitudinal-study-in-the-arthritispowe/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-treatment-and-disease-activity-with-antibiotic-use-and-hospitalized-infection-among-people-living-with-rheumatoid-arthritis-baseline-data-from-a-longitudinal-study-in-the-arthritispowe/