Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite the risk for poor outcomes and gaps in care in the transition from pediatric to adult care, most pediatric rheumatology centers lack formal pathways for transition. We evaluated preparation for transition with a validated quality measure in a single pediatric rheumatology center.
Methods: Patients 16 and older were sent the ADolescent Assessment of Preparation for Transition (ADAPT) survey via email. This quality measure assesses preparation for transition in three domains: (1) self-management, (2) prescription medications, and (3) transfer planning using specific questions about transition counseling received (Table 2). Responses were converted to composite scores and analyzed using descriptive statistics. The association of patient illness and demographic factors with composite transition scores were assessed using t-tests, ANOVA and linear regression. Logistic regression was used to evaluate for independent predictors of transition readiness.
Results: 78 of 337 patients completed the survey (response rate of 23%), of whom 77 had a visit within 1 year and were eligible to complete the assessment tool. Demographics and disease types are reported in Table 1.
Patients most frequently endorsed receiving counseling on taking charge of their health and remembering to take medications, but less than half reported receiving specific counseling about transitioning to an adult provider (Table 2).
Patients ages 16-18 had significantly lower scores in all domains as compared to those 19 years and older (Table 3). Patients with lower education attainment compared with those who had attended some college or higher had lower scores in self- management (1.51 vs 2.52, p=0.0002), prescription medication counseling (1.96 vs 2.41, p= 0.029), and transfer planning (0.27 vs 1.62, p< 0.001). Patients with a diagnosis of MCTD, Sjogrens or SLE had higher self-management scores than those with other diagnoses (2.6 vs 1.9; p=0.048). Non-white patients indicated they had received more thorough medication counseling than white patients (2.71 vs 2.07, p=0.027).
When controlling for age, educational attainment remained an independent predictor of transfer planning (Beta=1.00, 95% CI [0.06, 1.95], p=0.037), but not of other measures. Patients with longer duration of seeing their physician had higher transition preparation scores (r=0.26, p=0.021).
Conclusion: Few adolescents in our cohort endorsed receiving comprehensive transition counseling, including discussion of transfer planning. Patients who were younger and with lower levels of education had lower preparation scores. A long-term relationship with providers was associated with higher transition preparation scores. Further research including longitudinal assessment of transition preparation is needed to evaluate effective processes to assist vulnerable populations.
 Table 1. Patient Characteristics
Table 1. Patient Characteristics
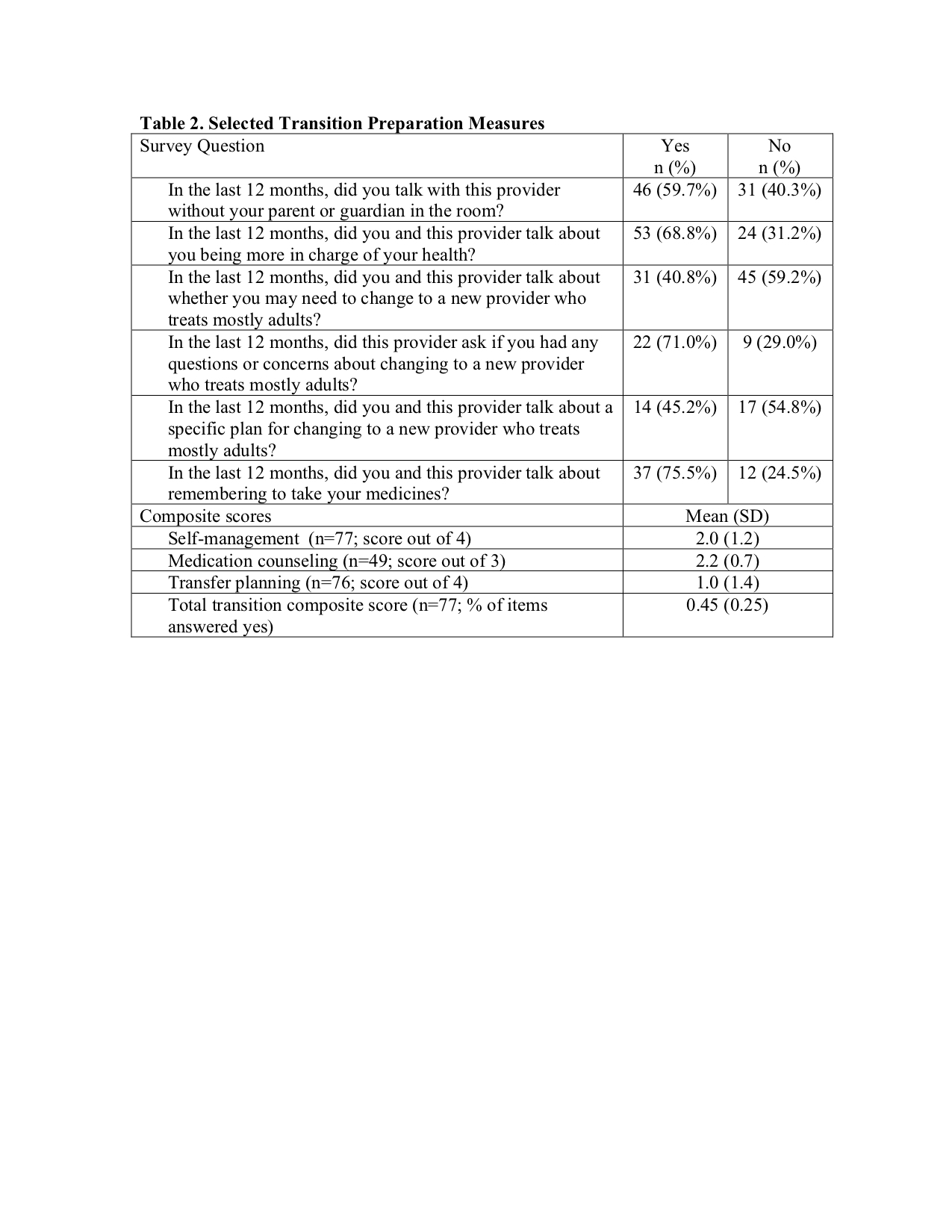 Table 2. Selected Transition Preparation Measures
Table 2. Selected Transition Preparation Measures
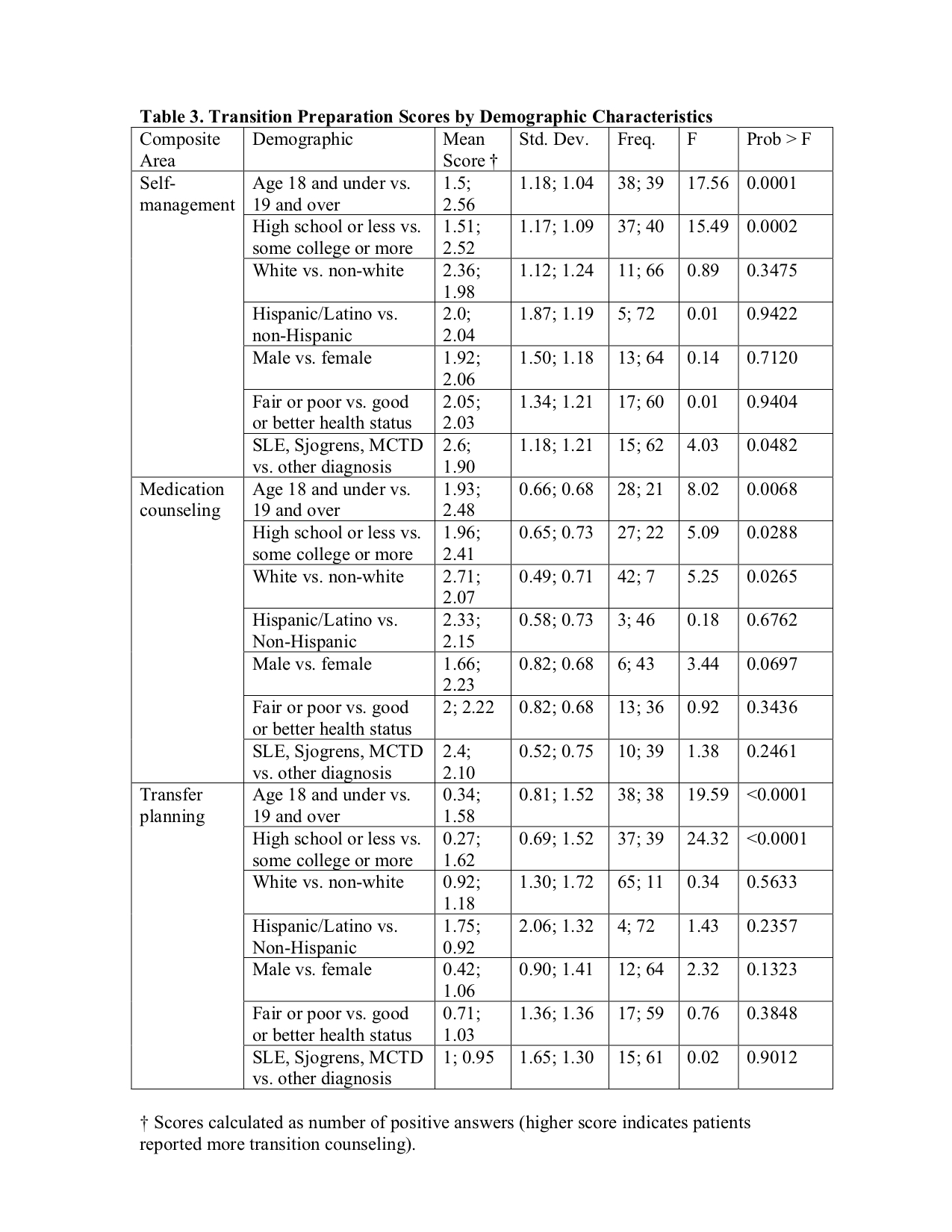 Table 3. Transition Preparation Scores by Demographic Characteristics
Table 3. Transition Preparation Scores by Demographic Characteristics
To cite this abstract in AMA style:
Roberts J, Halyabar O, Petty C, Son M. Assessing Preparation for Care Transition Among Adolescents with Rheumatologic Disease: A Quality Assessment with Patient Survey [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/assessing-preparation-for-care-transition-among-adolescents-with-rheumatologic-disease-a-quality-assessment-with-patient-survey/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-preparation-for-care-transition-among-adolescents-with-rheumatologic-disease-a-quality-assessment-with-patient-survey/
