Session Information
Date: Friday, November 6, 2020
Title: Patient Outcomes, Preferences, & Attitudes Poster I: RA, Spondyloarthritis, & OA
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Evidence-based guidelines for rheumatoid arthritis (RA) call for shared decision-making (SMD) as a method to personalize treatment decisions and achieve treat-to-target goals. We assessed alignment and discordances on treatment and SDM perceptions among RA patients and their rheumatology care teams.
Methods: Between 09/2019 and 06/2020, surveys were administered to RA patients and their health care professional (HCP) teams as part of in-clinic collaborative patient education sessions across 13 US-based rheumatology community practices. On 5-point Likert scales and multi-select questions, patients and HPs rated or indicated their perceptions, preferences, and concerns regarding RA treatment and SDM.
Results: Surveys were completed by 137 patients with RA (81% female, mean age 57 years) and 41 HCPs (52% physicians, 20% nurse practitioners, 4% physician assistants, 24% nurses) who reported 13 mean years of experience in rheumatology. Alignments were found in patients’ and HCPs’ perceptions of patients’ current level of RA control (well or very well controlled: 50% patients vs 58% HCPs) and satisfaction with current therapy (high or very high: 68% patients vs 65% HCPs).
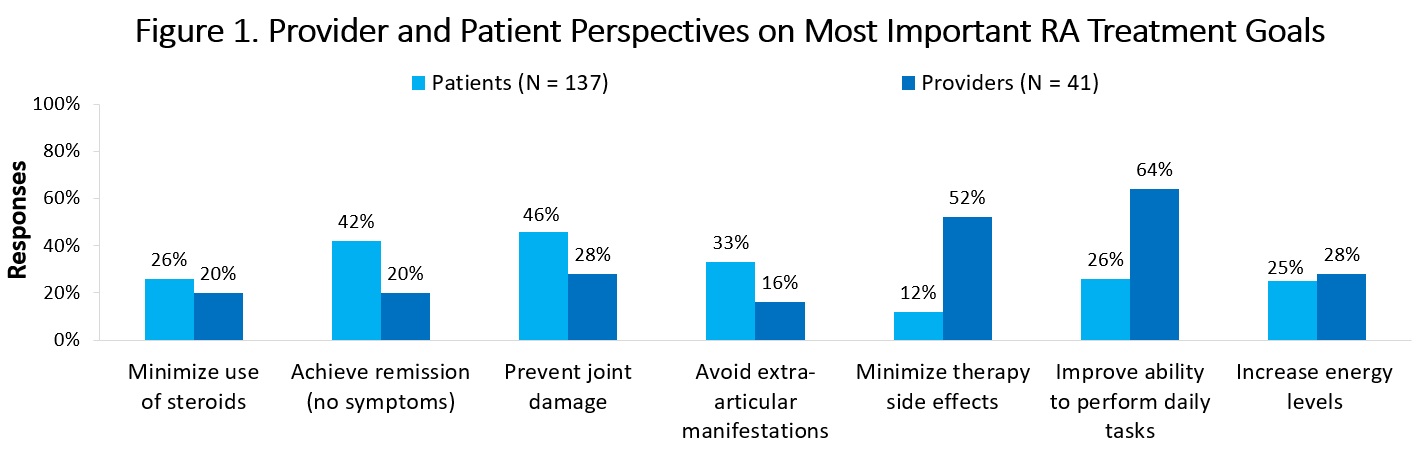
Discordances were found in patients’ and HCPs’ top goals for RA treatment (Figure 1), which included: prevent joint damage (46% patients, 28% HCPs), achieve remission (42% patients, 20% HCPs), avoid extra-articular manifestations (33% patients, 16% HCPs), improve ability to perform daily tasks (26% patients, 52% HCPs), and minimize therapy side effects (12% patients, 52% HCPs). Discordances were also observed in patients’ and HCPs’ main concerns about targeted therapy for RA (Figure 2), which included potential side effects (54% patients, 42% HCPs), efficacy (46% patients, 17% HCPs), cost (17% patients, 50% HCPs), and monitoring requirements (6% patients, 33% HCPs).
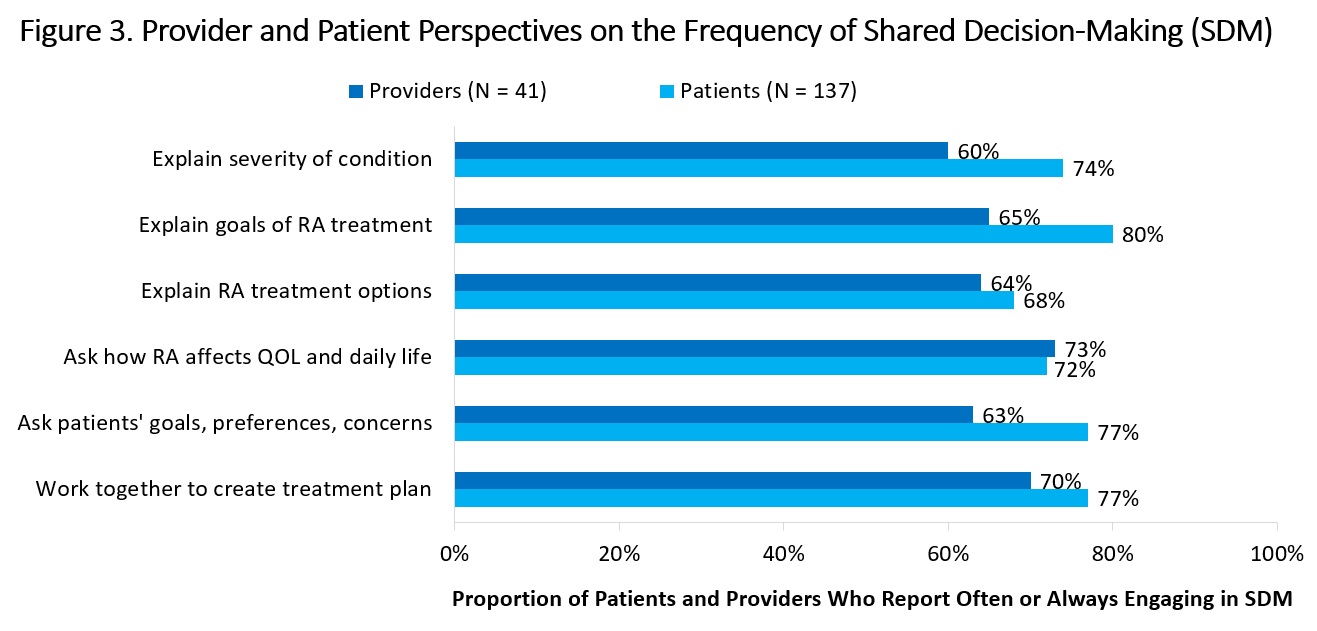
A high proportion of patients and HCPs reported often or always engaging in multiple components of SDM (Figure 3). However, compared with their patients’ responses, HCPs underestimated how often they: explain goals of treatment (80% patients; 65% HCPs), explain disease severity to patients (74% patients; 60% HCPs), and ask patients’ treatment goals, preferences, and concerns (77% patients; 63% HCPs). When asked about the main barrier to SDM, patients reported not knowing enough about RA and available therapies (46%) while HCPs reported perceived patient resistance to SDM (57%).
Conclusion: Identifying alignments and discordances in perceptions of treatment and SDM can support rheumatology teams in individualizing treatment decisions and patient engagement for optimal RA care.
To cite this abstract in AMA style:
Levin R, Parker C, Botsoglou K, Shah J, Dayal N, Fajardo K, Simone L, Carter J, Sapir T. Alignment and Discordances in Treatment Perceptions and Shared Decision-Making Among RA Patients and Rheumatology Care Teams [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/alignment-and-discordances-in-treatment-perceptions-and-shared-decision-making-among-ra-patients-and-rheumatology-care-teams/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/alignment-and-discordances-in-treatment-perceptions-and-shared-decision-making-among-ra-patients-and-rheumatology-care-teams/