Session Information
Date: Friday, March 31, 2023
Title: Poster Breakout 4 - JDM & Scleroderma: Clinical & Therapeutic Aspects
Session Type: Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: Juvenile dermatomyositis (JDM) is characterized by symmetric proximal muscle weakness, distinct rash, and a risk for calcinosis. Systemic immunosuppression is needed. Evidence is limited on the factors associated with disease remission off of medication. The aims of this study are to describe the demographic, clinical, laboratory, imaging characteristics in our JDM cohort, and to identify variables associated with medication-free remission.
Methods: This is a cross-sectional retrospective study of a convenience sample of children diagnosed with JDM at ≤18 years of age, with a minimum clinical follow-up of 2 years at Cincinnati Children’s Rheumatology Clinic. Medication-free remission was defined as inactive JDM off all systemic medications for at least 6 months. Medical records were reviewed. We compared the following variables in children who achieved remission to those who did not: demographics, clinical features, muscle enzymes, ANA, myositis-specific auto-antibodies, Childhood Myositis Assessment Scale (CMAS) scores, and physician, parent and patient global assessment scores. Group differences were tested using Fisher’s Exact tests and Wilcoxon Rank Sum tests. A p< 0.05 was considered statistically significant. Analysis was conducted using SAS 9.3©.
Results: Of 70 participants, 47 (67%) achieved medication-free remission while 23 (33%) were still on medication at last follow-up. Overall, most were Non-Hispanic White (87%), females (64%), had a median age of JDM onset 5 years (range 3-11), and median age of diagnosis of JDM of 5 years (4-11). Those who achieved medication-free remission required treatment for 43 (interquartile [IQR] 28-77) months before discontinuation. They were of a younger median age at JDM onset (5 [IQR 3-6] vs 9 [5-12] years) and JDM diagnosis (5 [3-7] v. 9 [5-12] years) compared to those who did not achieve remission. Males were less likely to achieve remission (28% [n=13] in remission vs. 52% [12], p=0.044). Both groups had similar presentation of rash, muscle weakness, elevated muscle enzyme levels, ANA positivity, abnormal muscle and skin biopsy, and MRI findings (in those who had them done). Time to treatment initiation was similar, and prednisone (94%), methotrexate (87%) and IVIG (56%) were most commonly prescribed. Children unable to achieve medication-free remission were more likely to be on IVIG (74% [17/39], p=0.032), tofacitinib (100% [3/3], p=0.032), and abatacept (22% [5/7], p=0.030). At last follow up, they also had worse patient/parent scores global assessment scores (0.0 [0-1.5] vs 1.0 [0-5.0], p=0.012), but similar CMAS and physician global scores (Table 3).
Conclusion: Although 2/3 of patients achieved medication-free remission, 1/3 of our cohort remained on treatment. Sex and age may be important factors as more children who were males and older at JDM onset/ diagnosis were less likely to achieve medication-free remission. These children were also found to be on tofactitinib, IVIG, and abatacept.
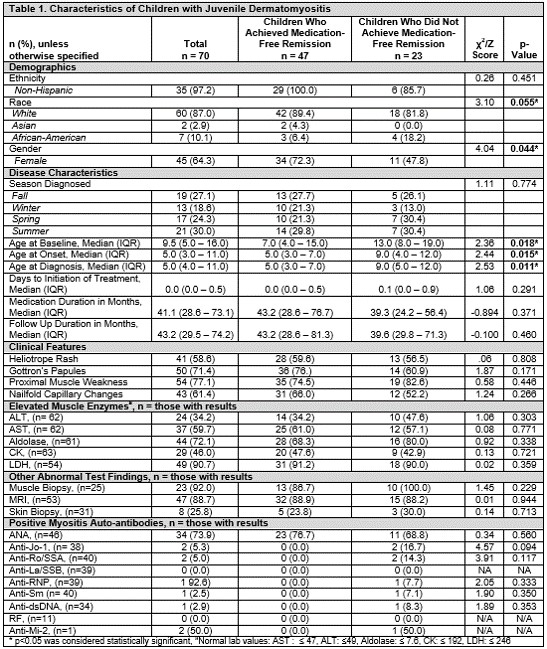 Table 1. Characteristics of Children with Juvenile Dermatomyositis
Table 1. Characteristics of Children with Juvenile Dermatomyositis
 Table 2. Medication Administration in Management of Juvenile Dermatomyositis
Table 2. Medication Administration in Management of Juvenile Dermatomyositis
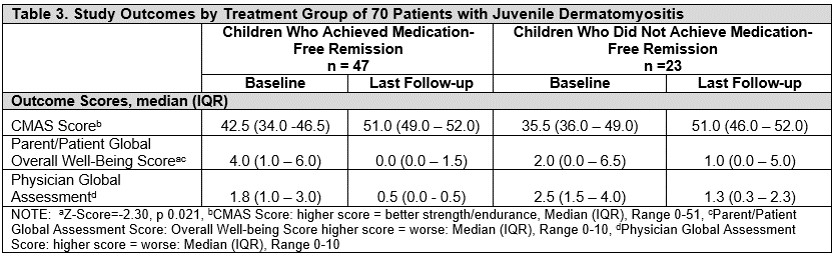 Table 3. Study Outcomes by Treatment Group of 70 Patients with Juvenile Dermatomyositis
Table 3. Study Outcomes by Treatment Group of 70 Patients with Juvenile Dermatomyositis
To cite this abstract in AMA style:
Ghumman H, Maccora I, Brunner H, Cassedy A, Altaye M, Firdous A, Grom A, Lovell D, Merritt A, Quinlan-Waters M, Angeles-Han S. Achieving Medication-Free Remission in Juvenile Dermatomyositis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/achieving-medication-free-remission-in-juvenile-dermatomyositis/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/achieving-medication-free-remission-in-juvenile-dermatomyositis/
