Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Lipodermatosclerosis (LDS) is a progressive manifestation of chronic venous insufficiency characterized by distinctive lower extremity changes, including an “inverted champagne bottle” appearance, skin hyperpigmentation, and occasionally, non-healing ulcers. (see Figure 1) While LDS is not extensively studied in the context of connective tissue diseases, it shares similar pathogenic pathways with systemic sclerosis (SSc), where vasculopathy leads to tissue hypoxia, inflammation, and subsequent fibrosis of the skin and subcutaneous tissues. This study estimated the prevalence of LDS in SSc, examined the demographic and SSc-related characteristics of patients with LDS, and estimated the association between LDS and major vascular outcomes in patients with SSc.
Methods: We performed a retrospective cohort analysis of adult patients who had prospectively enrolled in our Autoimmune Skin Disease Registry between 2004-2023 and met ACR/EULAR 2013 classification criteria for SSc. Descriptive statistics were used to summarize data, and chi-square/Fisher’s exact test and t-test/Mann-Whitney U test were employed to compare categorical and continuous variables, respectively. Logistic regression estimated prevalence odds ratios (pOR) and 95% confidence intervals of the association between LDS and a composite macrovascular outcome measure, including digital gangrene and/or renal crisis and/or pulmonary hypertension, adjusted for age and follow-up time. A. sensitivity analysis was conducted for the outcome of pulmonary hypertension (PH).
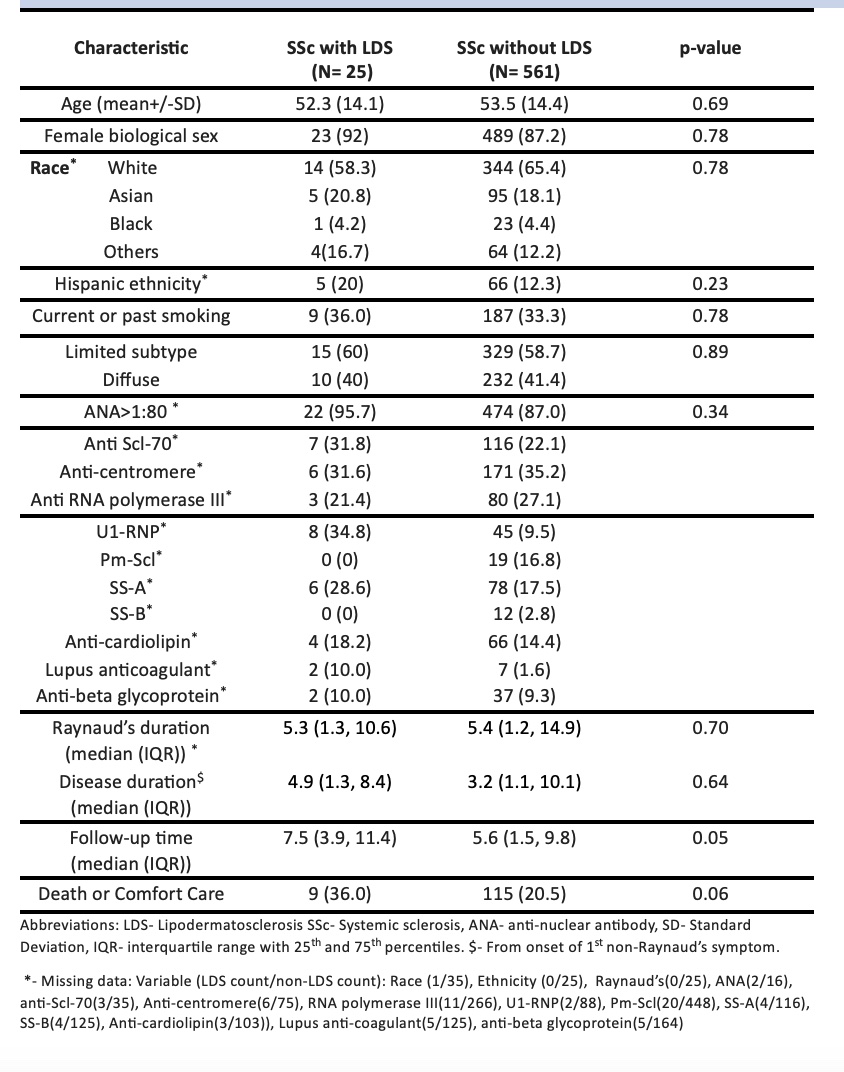
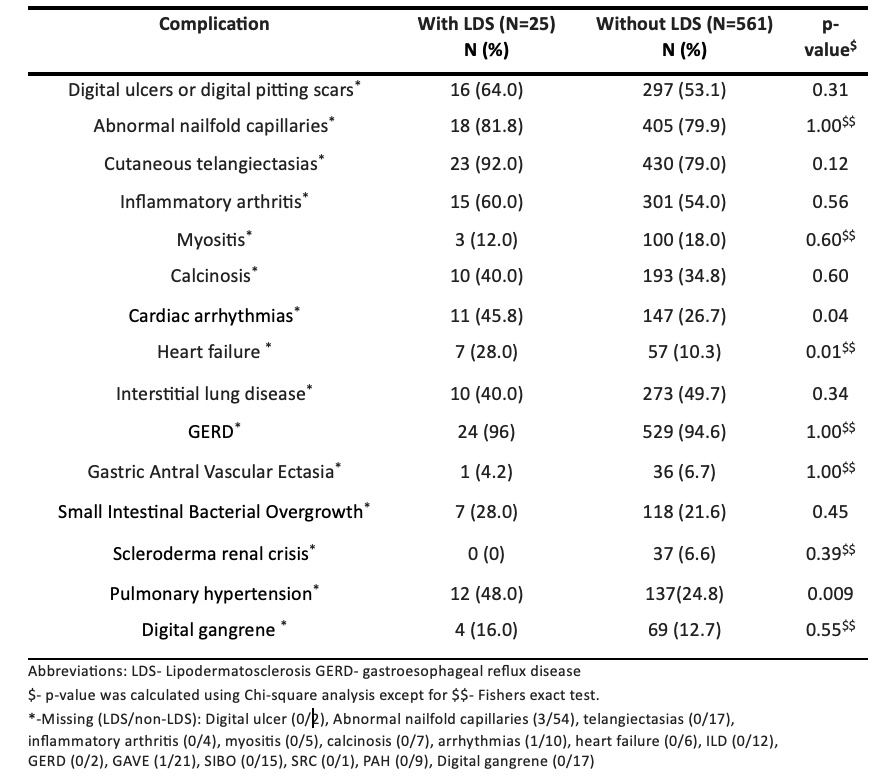
Results: Among 586 SSc patients, 4% (N=25) had LDS. Baseline demographic and disease features were similar between patients with and without LDS (Tables 1 and 2) with the exception that patients with LDS had higher frequencies of cardiac arrhythmias, heart failure, and PH. Among patients with LDS, 36% were either discharged to hospice or died during a median follow-up time of 7.5 (IQR- 3.9, 11.4) years, compared to 20.5% of patients without LDS followed for 5.6 (IQR-1.5, 9.8) years. LDS was associated with the composite vascular outcome in adjusted analysis with pOR=2.36 [1.02-5.45], but this was primarily driven by the association with PH. Sensitivity analysis confirmed an elevated pOR between LDS and pulmonary hypertension, with an adjusted pOR of 3.20 [1.37-7.49].
Conclusion: LDS was diagnosed in 4% of SSc patients evaluated at a multi-disciplinary Rheumatologic Dermatology Clinic. Patients with LDS have more than two-fold higher prevalence of a composite macrovascular outcome and more than three-fold higher prevalence of pulmonary hypertension. We conclude that LDS could portend severe vasculopathic manifestations in SSc, however, temporality could not be determined by our analyses. Clinicians should recognize the clinical features of LDS in SSc patients and closely monitor these patients for PH and other macrovascular complications.
To cite this abstract in AMA style:
Davuluri S, Kapoor P, Nandyala S, Fiorentino D, Simard J, Chung L. A Novel Association Between Lipodermatosclerosis and Key Vascular Outcomes in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-novel-association-between-lipodermatosclerosis-and-key-vascular-outcomes-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-novel-association-between-lipodermatosclerosis-and-key-vascular-outcomes-in-systemic-sclerosis/