Session Information
Date: Tuesday, October 28, 2025
Title: (2437–2469) Systemic Lupus Erythematosus – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic autoimmune disease linked to significant morbidity, including pulmonary hypertension (PH). While SGLT2 inhibitors are known for cardiovascular and renal benefits, their impact on PH in SLE remains underexplored. This study assesses the association between SGLT2 inhibitor use and reduced risks of PH, mortality, and other cardiopulmonary outcomes in SLE patients.
Methods: This retrospective cohort study utilized the TriNetX Research Network to identify two cohorts of SLE patients—those prescribed SGLT2 inhibitors and non-users—between August 1, 2014, and August 1, 2024. SLE patients were identified using ICD-10 codes. Outcomes, including pulmonary hypertension (PH), mortality, hospitalizations, and lupus nephritis, were also defined using ICD-10 codes and additional codes available on the TriNetX platform. Data analysis was performed in January 2025.Propensity score matching (PSM) in a 1:1 ratio was applied to achieve balanced baseline characteristics between the two cohorts, including demographics, steroid use, comorbidities, and SLE-specific laboratory markers. Following matching, outcomes were compared between the two groups over a follow-up period of five years. Statistical analysis was conducted using Cox proportional hazards models for time-to-event outcomes, Kaplan-Meier survival curves for visualizing survival differences, and log-rank tests to assess statistical significance between the matched cohorts.
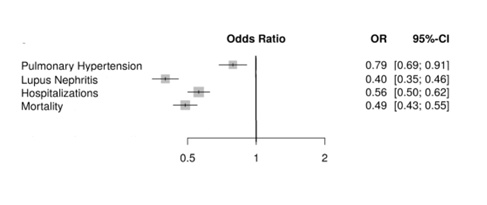
Results: After propensity score matching, 7,556 patients were included in each cohort, ensuring balanced demographics (mean age: 61 years, 80% female, 46% White). SGLT2 inhibitor use was associated with a significantly lower incidence of pulmonary hypertension (PH) (5.7% vs. 7.1%; OR: 0.79, 95% CI: 0.69–0.91; p < 0.001).All-cause mortality was reduced in the SGLT2i group (5.8% vs. 11.2%; OR: 0.49, 95% CI: 0.43–0.55; p < 0.001), and hospitalizations were less frequent among SGLT2i users (27.9% vs. 40.8%; OR: 0.56, 95% CI: 0.50–0.63; p < 0.001). Additionally, SGLT2i use was associated with a significantly lower incidence of lupus nephritis (4.9% vs. 11.4%; OR: 0.40, 95% CI: 0.35–0.46; p < 0.001).
Conclusion: SGLT2 inhibitors were significantly associated with reduced risk of PH, mortality, lupus nephritis, and other cardiopulmonary complications in SLE patients. These findings support the potential role of SGLT2 inhibitors as an adjunctive therapy in SLE management. Prospective studies are warranted to confirm these results.
.jpg) Table 1: Summary of primary and secondary outcomes with odds ratios and p-values.
Table 1: Summary of primary and secondary outcomes with odds ratios and p-values.
.jpg) Forest plot summarizing odds ratios and 95% CIs for all primary and secondary outcomes.
Forest plot summarizing odds ratios and 95% CIs for all primary and secondary outcomes.
To cite this abstract in AMA style:
Alomari A, Khanfar A, Rodriguez M, Alawneh D. SGLT2 Inhibitors in SLE: Impact on Pulmonary Hypertension, Mortality, and Renal Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/sglt2-inhibitors-in-sle-impact-on-pulmonary-hypertension-mortality-and-renal-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sglt2-inhibitors-in-sle-impact-on-pulmonary-hypertension-mortality-and-renal-outcomes/