Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoarthritis (OA) is a leading cause of disability worldwide, characterized by progressive joint degeneration, chronic pain and functional impairment (PMID: 24024017). While imaging modalities such as radiographs are standard for OA diagnosis, emerging research suggests that ultrasound (US) imaging, potentially in combination with other disease markers such as soluble biomarkers and cytokines, may offer a more dynamic assessment of joint health (PMID: 39201072). This study aims to explore these associations utilizing data from the Johnston County Health Study (JoCoHS), a population-based cohort initiated in 2019 in North Carolina.
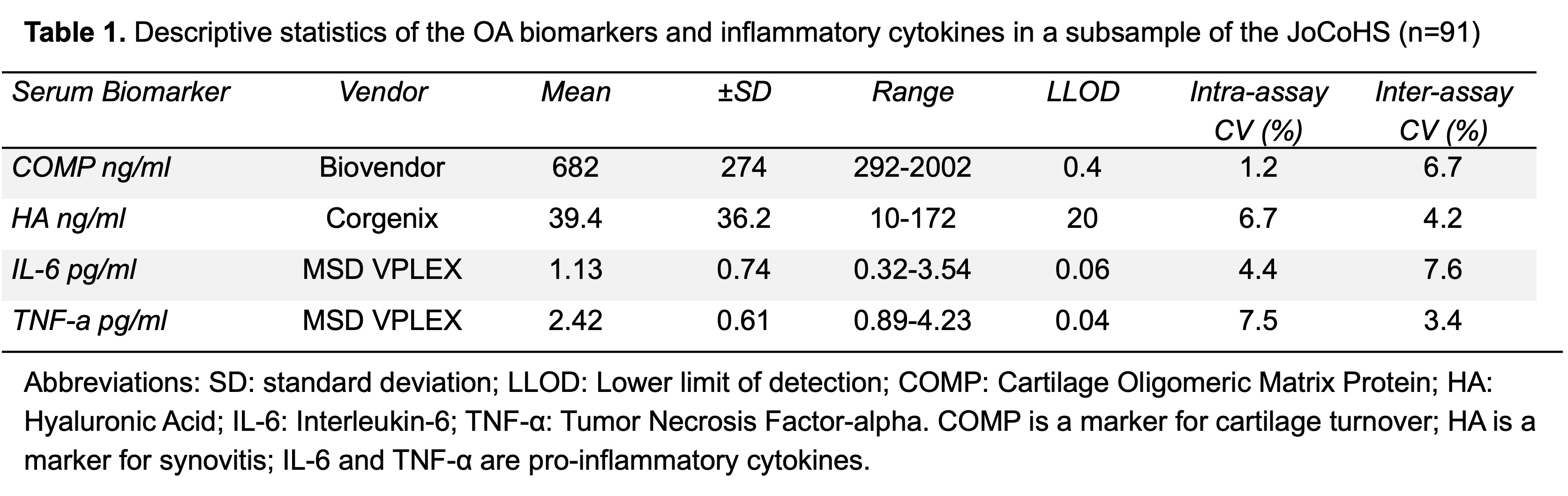
Methods: Participants (Nf91) in JoCoHS who underwent bilateral knee US and serum and plasma biomarker assessment by ELISA as part of a substudy (Table 1) were included. US images were acquired by a trained sonographer and scored by two expert readers using standardized criteria for distinct structural and inflammatory joint pathologies including synovitis, osteophytes, meniscal and cartilage damage (Table 2, described in PMID 39989271). Separate linear regression models of associations between each log-transformed biomarker with each US feature were used to produce adjusted mean differences (betas) and 95% confidence intervals (CI), adjusted for age, sex, race/ethnicity, body mass index (BMI), education (as a proxy for socioeconomic status), Charlson Comorbidity index (CCI), and symptoms in other sites (i.e., hip, wrist, or hand).
Results: Among 91 participants (mean age 55 [range 35-70] years, 39% male, 35% Black, 12% Hispanic, mean BMI 34 kg/m2) with US and biomarker data, joint pathology and GS synovitis were common, with 92% of participants having at least one knee with cartilage damage on US. On average, elevated cartilage oligomeric matrix protein levels (COMP) were modestly but significantly associated with the presence of mild medial osteophytes (Table 2). Hyaluronic acid (HA) levels were significantly higher in participants with severe effusion/synovitis, severe GS synovitis, and medial meniscal extrusion. Increased interleukin-6 (IL-6) levels were observed in association with both PD synovitis and lateral cartilage damage. Both HA and IL-6 were higher in those with severe medial cartilage damage, but this was not statistically significant. Additionally, tumor necrosis factor-alpha (TNF-a) levels were on average slightly higher in individuals with severe GS synovitis, lateral osteophytes and medial meniscal extrusion (Table 2).
Conclusion: Our findings demonstrate that specific US features of joint pathology relevant to OA are associated with distinct biomarkers in a diverse population, particularly HA and GS synovitis, which had the strongest associations. These results support the role of structural changes and inflammation in the pathogenesis of OA and highlight the utility of US imaging (which allows visualization of soft tissues in a more accessible manner than does MRI) and biomarker data for characterizing disease variation and tailored avenues of assessment, monitoring and treatment.
To cite this abstract in AMA style:
Kimber J, Alvarez C, Kraus V, Huebner J, Arbeeva L, Schwartz T, Golightly Y, Loeser R, Nelson A. Associations Among Biomarkers, Cytokines, and Ultrasound Features of Knee Osteoarthritis: A Cross-Sectional Analysis in the Johnston County Health Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/associations-among-biomarkers-cytokines-and-ultrasound-features-of-knee-osteoarthritis-a-cross-sectional-analysis-in-the-johnston-county-health-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-among-biomarkers-cytokines-and-ultrasound-features-of-knee-osteoarthritis-a-cross-sectional-analysis-in-the-johnston-county-health-study/

.jpg)