Session Information
Date: Monday, October 27, 2025
Title: (1248–1271) Patient Outcomes, Preferences, & Attitudes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Pulmonary disease is present in most sarcoidosis cases with up to 10% of patients progressing to advanced lung disease.1 Pulmonary sarcoidosis accounted for 2.5% of lung transplants in 2015. Idiopathic pulmonary fibrosis (IPF) is a much more common indication for lung transplantation.2 Post-transplant outcomes for both indications are presumed to be comparable.1,2 The current study evaluates the experience and outcomes across multiple sites at a single institution.
Methods: All lung transplants occurring at any site between July 2017 and March 2023 were reviewed. Descriptive statistics were performed and compared between pulmonary sarcoidosis and IPF indications via Kruskal-Wallis and Fischer’s Exact tests. Survival and pulmonary function test results were compared between groups. Kaplan-Meier curves and hazard ratios were used for survival comparison.
Results: Lung transplantation outcomes for 13 cases of sarcoidosis were compared to 26 age- and gender-matched IPF cases. The most common computed tomography pattern was usual interstitial pneumonia (61.5%) in the IPF group compared to undefined pattern (38.5%) in the sarcoidosis group. Baseline characteristics were otherwise comparable (Table 1). A higher proportion of sarcoidosis patients had improved post-transplant forced vital capacity compared to IPF patients although this difference was not statistically significant (Figure 1). Survival plateaued at 75% in both groups after 5 years with hazard ratio 0.56 (p=0.49) (Figure 2).
Conclusion: Lung transplantation is a feasible treatment strategy for pulmonary sarcoidosis and demonstrated comparable outcomes to IPF in this cohort. Rheumatologists treating sarcoidosis can therefore benefit from familiarity with current lung transplantation referral guidelines, disease-specific indications and contraindications, and multidisciplinary collaboration.Kim JS, Gupta R. Lung transplantation in pulmonary sarcoidosis. J Autoimmun. 2023;149:103135. doi:10.1016/j.jaut.2023.103135Yusen RD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-second official adult lung and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant. 2015;34(10):1264-1277. doi:10.1016/j.healun.2015.08.014
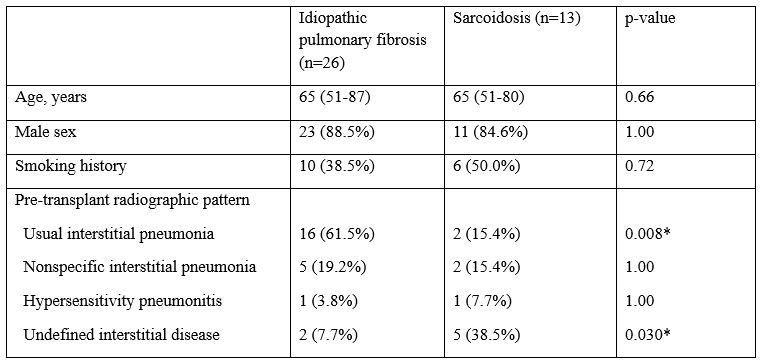 Table 1. Baseline (pre-transplant) characteristics of idiopathic pulmonary fibrosis and sarcoidosis groups. Statistically significant differences are designated by an asterisk (*).
Table 1. Baseline (pre-transplant) characteristics of idiopathic pulmonary fibrosis and sarcoidosis groups. Statistically significant differences are designated by an asterisk (*).
.jpg) Figure 1. Forced vital capacity (FVC) pre- and post-transplant compared between sarcoidosis and idiopathic pulmonary fibrosis (IPF) groups. FVC scores were categorized as normal (>80%), mildly reduced (60-80%), moderately reduced (50-60%), and severely reduced ( < 50%). Missing data points were excluded from proportion calculations. Differences were not statistically significant.
Figure 1. Forced vital capacity (FVC) pre- and post-transplant compared between sarcoidosis and idiopathic pulmonary fibrosis (IPF) groups. FVC scores were categorized as normal (>80%), mildly reduced (60-80%), moderately reduced (50-60%), and severely reduced ( < 50%). Missing data points were excluded from proportion calculations. Differences were not statistically significant.
.jpg) Figure 2. Kaplan-Meier survival curve demonstrating comparable post-transplant survival between idiopathic pulmonary fibrosis (red) and sarcoidosis (blue) groups.
Figure 2. Kaplan-Meier survival curve demonstrating comparable post-transplant survival between idiopathic pulmonary fibrosis (red) and sarcoidosis (blue) groups.
To cite this abstract in AMA style:
Yaman R, Balistreri L, Diaz Menindez M, Mumtaz S, Sullivan M, Hochwald A, Berianu F. Lung Transplantation Outcomes for Pulmonary Sarcoidosis Compared to Idiopathic Pulmonary Fibrosis: A Single Institution Multisite Experience [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/lung-transplantation-outcomes-for-pulmonary-sarcoidosis-compared-to-idiopathic-pulmonary-fibrosis-a-single-institution-multisite-experience/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lung-transplantation-outcomes-for-pulmonary-sarcoidosis-compared-to-idiopathic-pulmonary-fibrosis-a-single-institution-multisite-experience/
