Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Heart failure (HF) is a major cause of morbidity and mortality in rheumatoid arthritis (RA). Prior work has suggested that higher levels of inflammation is associated with increased future risk of HF. Several inflammatory pathways are hypothesized to play a role in both RA and HF including interleukin-1-beta (IL-1b), interleukin-6 (IL-6), and soluble tumor necrosis factor-2 (sTNFR2). The Predicting Risk of Cardiovascular Disease Events (PREVENT) risk equation published in 2023 includes a validated risk estimator for predicted 10-year HF risk (PREVENT-HF). The objective of this study was to determine the cross-sectional association between inflammatory biomarkers and predicted HF risk in RA to identify potential markers of HF risk in RA.
Methods: We studied patients from the LiiRA (Lipids, Inflammation and Cardiovascular risk in RA) study, who had active RA with a plan to initiate tumor necrosis factor inhibitor (TNFi) therapy. All patients underwent measurements for high-sensitivity C-reactive protein (hsCRP), erythrocyte sedimentation rate (ESR), IL-1b, IL-6, sTNFR2, NT-pro-BNP, and high sensitivity cardiac troponin (hs-cTnT) at the baseline visit. We calculated the estimated risk of HF for each patient at baseline using PREVENT-HF risk equations. Spearman’s correlation was calculated for each biomarker value and the PREVENT-HF score. We performed a univariable linear regression to determine the association between detectable hs-cTnT ( >6ng/L) and PREVENT-HF score. Biomarkers significantly correlated with PREVENT-HF score (p< 0.05) in the univariable analyses were considered in a multivariable linear regression testing the association with PREVENT-HF score, adjusting for RA disease duration and disease activity (PREVENT-HF includes age and sex).
Results: We studied 73 patients, 82% female, median age 56 years (Table 1). The median RA duration at baseline was 3.6 years and median CDAI was 22 (moderate disease activity). The median PREVENT-HF 10-year estimated HF risk was 2.1% (IQR 0.7, 5.1), and 21% of the cohort had a detectable hs-cTnT. Higher levels of hsCRP, ESR, IL-6, and sTNFR2 were correlated with higher PREVENT-HF estimated HF risk, and detectable hs-cTnT was associated with higher PREVENT-HF estimated HF risk (Table 2). Starting with a model including inflammatory markers measured in clinic (ESR and hsCRP), sTNFR2 was associated with PREVENT-HF risk after adjustment for these inflammatory biomarkers, RA duration, and disease severity (Table 3). The addition of hs-cTnT to the model attenuated the association between sTNFR2 and estimated HF risk, and ESR maintained a significant association with estimated HF risk. Adjusting for NT-pro-BNP did not change the associations.
Conclusion: In this RA cohort with moderate disease activity, among candidate inflammatory markers, ESR and sTNFR2 were most correlated with higher PREVENT-HF risk scores. Moreover, detectable hs-cTnT was most strongly associated with higher PREVENT-HF risk scores. More studies are needed to further examine specific inflammatory pathways, e.g., TNF, and subclinical myocardial injury as potential markers of HF risk in RA.
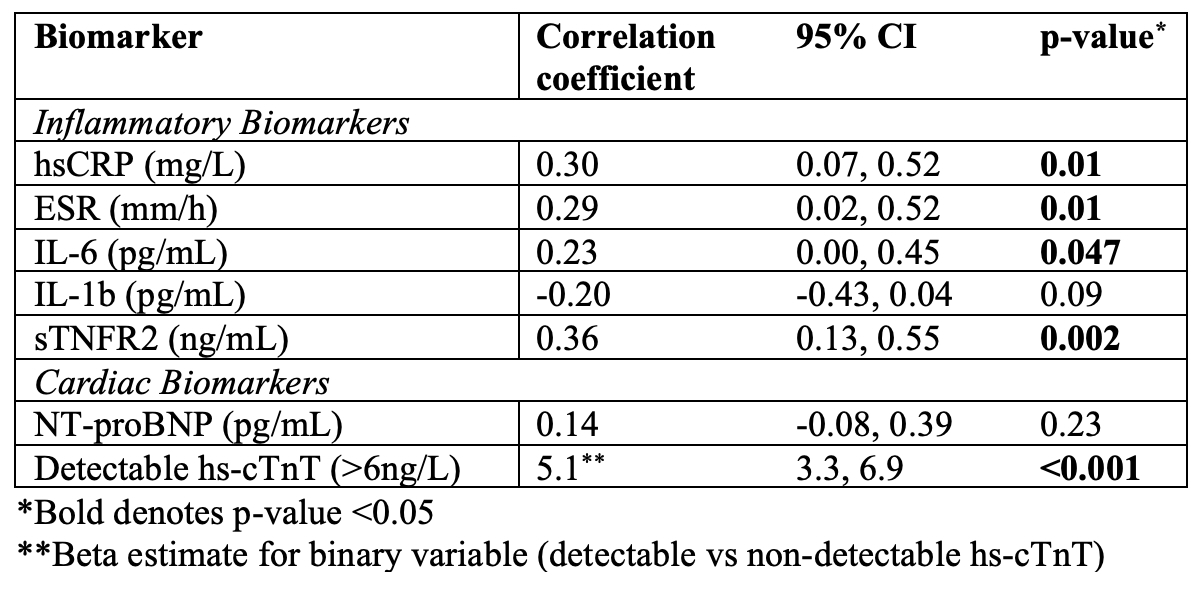 Table 1. Baseline characteristics for LiiRA cohort (n=73)
Table 1. Baseline characteristics for LiiRA cohort (n=73)
.jpg) Table 2. Correlation between inflammatory and cardiac biomarkers and PREVENT-HF risk
Table 2. Correlation between inflammatory and cardiac biomarkers and PREVENT-HF risk
.jpg) Table 3. Multivariable linear regressions for the association between cardiac and inflammatory biomarkers and PREVENT-HF risk
Table 3. Multivariable linear regressions for the association between cardiac and inflammatory biomarkers and PREVENT-HF risk
To cite this abstract in AMA style:
Usiskin I, rusnak L, Zhong K, Qi Y, Yang N, McDermott G, Weber B, Liao K. Association between inflammatory biomarkers and predicted heart failure risk in rheumatoid arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-between-inflammatory-biomarkers-and-predicted-heart-failure-risk-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-inflammatory-biomarkers-and-predicted-heart-failure-risk-in-rheumatoid-arthritis/
