Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Medications used to manage juvenile idiopathic arthritis (JIA) are highly effective in preventing joint damage and provide a favorable prognosis. Many patients, however, struggle with treatment adherence. Yet, little data exist on self-reported medication barriers and how they may affect treatment adherence and disease activity in this vulnerable population.
Methods: Retrospective cross-sectional analysis was used to examine medication barriers in a cohort of patients with JIA seen in an ambulatory rheumatology clinic at a quaternary care academic institution in Charleston, SC. Pediatric Rheumatology Care and Outcomes Improvement Network Barriers Assessment Tool (BAT) was used to obtain patient/caregiver-reported medication barriers. Treatment adherence rates were estimated using a patient/caregiver-driven survey. 10-point clinical Juvenile Arthritis Disease Activity Score (cJADAS-10) assessed disease activity. Primary objectives were to investigate relationships among medication barriers, medication adherence, and disease activity. Secondary objective was to evaluate for health disparities associated with medication barriers. Fisher’s exact or Wilcoxon rank-sum tests were used to make between-group comparisons.
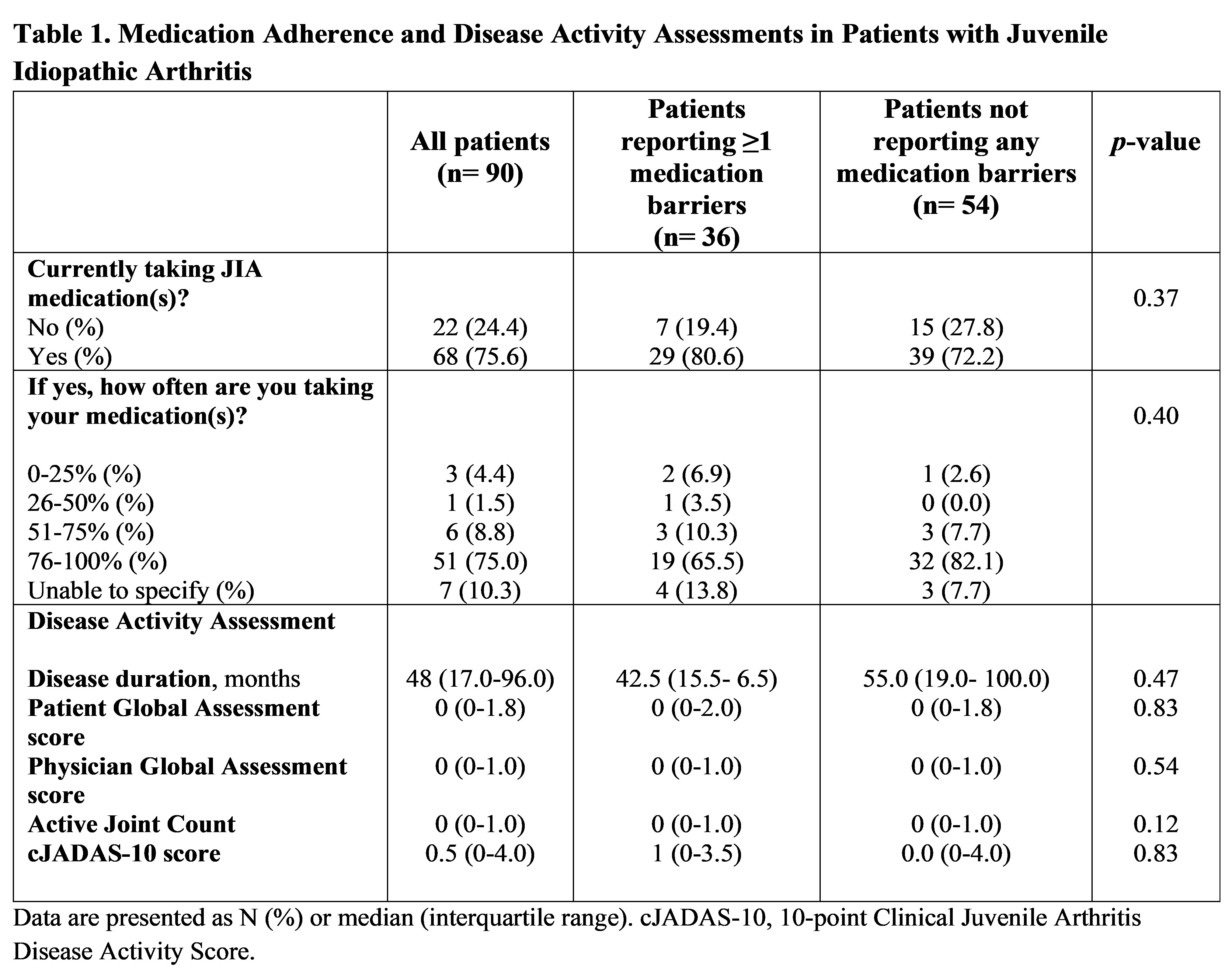
Results: 90 patients were included (median age 14 years; 73.3% female); 75.6% reported taking ≥1 JIA medication. 36 of 90 patients (40%) reported the presence of at least one medication barrier; 54 (60%) reported not having any barriers. “Treatment is painful,” “treatment makes me uncomfortable or upset,” and “I do not like the side effects of the treatment” were the most reported barriers. Comparison groups were based on the selection of one or more medication barriers from the BAT in primary analysis; and on the response to the survey question “Do you have any barriers to, challenges with, or concerns about taking your medication(s)?” in secondary analysis. Associations between medication barriers and medication adherence rates, disease activity and sociodemographic variables were not statistically significant in the primary analysis (Tables 1 & 2). However, medication barriers were found to decrease adherence rates in the secondary analysis with a different operational definition of medication barriers (Table 3).
Conclusion: No differences were observed in treatment adherence rates, disease activity and sociodemographic factors in patients reporting medication barriers versus not reporting any barriers. However, medication adherence varied with different operational definitions of medication barriers. Hence, additional investigation is warranted to further delineate perceived medication barriers and their effects on long-term disease outcomes.
To cite this abstract in AMA style:
Shaily A, Eckard A, Nietert P, Vara E, Ruth N, Gilbert M. Effects of Self-Reported Medication Barriers on Medication Adherence and Disease Activity in a Cohort of Patients with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/effects-of-self-reported-medication-barriers-on-medication-adherence-and-disease-activity-in-a-cohort-of-patients-with-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effects-of-self-reported-medication-barriers-on-medication-adherence-and-disease-activity-in-a-cohort-of-patients-with-juvenile-idiopathic-arthritis/

.jpg)
.jpg)