Session Information
Date: Sunday, October 26, 2025
Title: (0210–0232) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Geriatric integrative care models, such as the Perioperative Optimization of Senior Health (POSH) initiative, have shown improved outcomes (PMID: 29299599), yet there remains limited adoption in specialty clinics such as Rheumatology. This study aims to assess the findings of a novel Geri-Rheumatology clinic by a dual rheumatologist-geriatrician at an academic medical center. To test our hypothesis that an interplay of chronic inflammation and cardiovascular disease (CVD) risks impact rheumatology patients who have been shown to have higher rates of cognitive impairment (PMID: 39542002), we aimed to evaluate associated risk factors in older patients compared to peers without inflammatory conditions.
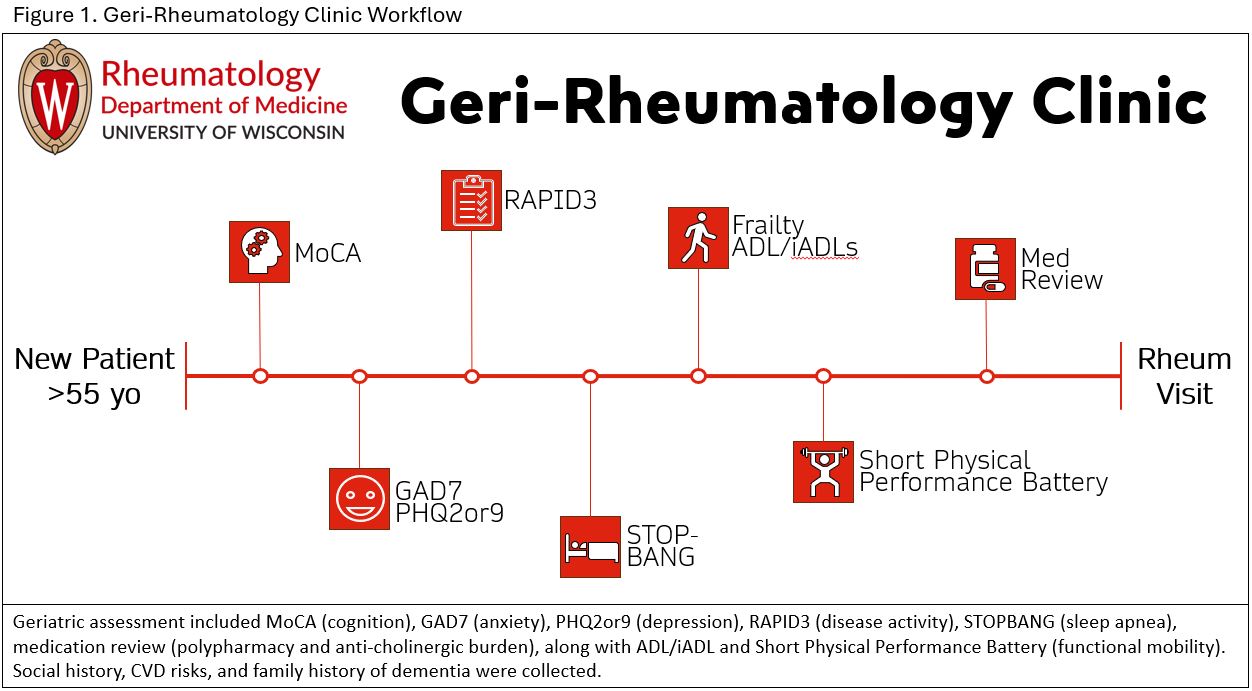
Methods: In this quality improvement pilot from August 2023 through November 2025, new Geri-Rheumatology referrals for ages >55 years were offered a geriatric evaluation using validated screening tools performed by Montreal Cognitive Assessment (MoCA) certified practitioners preceding their rheumatology visit (Figure1). The 5M’s of Geriatrics were integrated through clinical assessments of Mobility (Short Physical Performance Battery [SPPB]), Mind (MoCA), Medications (polypharmacy and anti-cholinergic burden), Multicomplexity (medical and social history assessment), and Matters Most, by appropriate counseling and referrals. Patients could opt-in to the full geriatric assessment or certain elements. Cognitive risk factors of sleep apnea, depression, anxiety, and disease activity were assessed along with CVD medical history. Patients with primary diagnosis codes for rheumatologic diseases (ex. SLE, RA) were compared to those with non-inflammatory codes (ex. OA, Positive ANA, Osteoporosis).
Results: A total of 77 patients completed a MOCA assessment and are included in this evaluation. With a cut off for Cognitive Impairment of ≤25, 35% (27) showed cognitive impairment with 3.9%(3) showing moderate impairment. While cognitive impairment frequencies were similar between rheumatologic and non-inflammatory cohorts, rheumatologic patients had higher baseline rates of CVD comorbidities (Table1). Lower MOCA scores were similar between cohorts and inversely related to age. The most common impairments were in Visuospatial, Attention, and Recall domains (Table2).Polypharmacy (≥ 5 medications) was found in 73% vs 62% (p=0.44) of the rheumatologic and non-inflammatory cohorts, respectively. The average overall anti-cholinergic burden was 2.2 medications. The geriatric assessment led to 24 memory clinic, 12 physical therapy, and 15 sleep study referrals.
Conclusion: With a growing geriatric population, this study adds to the body of knowledge informing care for older rheumatology patients. Nearly 1/3 of patients were offered referral to memory clinic for further evaluation. Clinicians should consider cognitive screening for this high-risk group as dementia affects patient outcomes, counseling, and medication adherence. Limitations were small cohort size and that patients self-selected involvement; no patients had severe impairment likely due to difficulties with visit attendance or consent. Future studies should expand this cohort to evaluate long-term outcomes.
To cite this abstract in AMA style:
Levinson J, Bartels C. Integration of the 5Ms of Geriatrics in a Novel Geri-Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/integration-of-the-5ms-of-geriatrics-in-a-novel-geri-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/integration-of-the-5ms-of-geriatrics-in-a-novel-geri-rheumatology-clinic/

.jpg)
.jpg)