Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: RA-associated lung disease (RA-LD), including RA-associated interstitial lung disease (RA-ILD) and RA-associated bronchiectasis (RA-BR), is a serious extra-articular manifestation of RA that significantly contributes to morbidity and mortality. Although previous studies have documented the adverse clinical outcomes associated with RA-LD, its impact on hospitalization risk is insufficiently investigated, particularly for RA-BR.
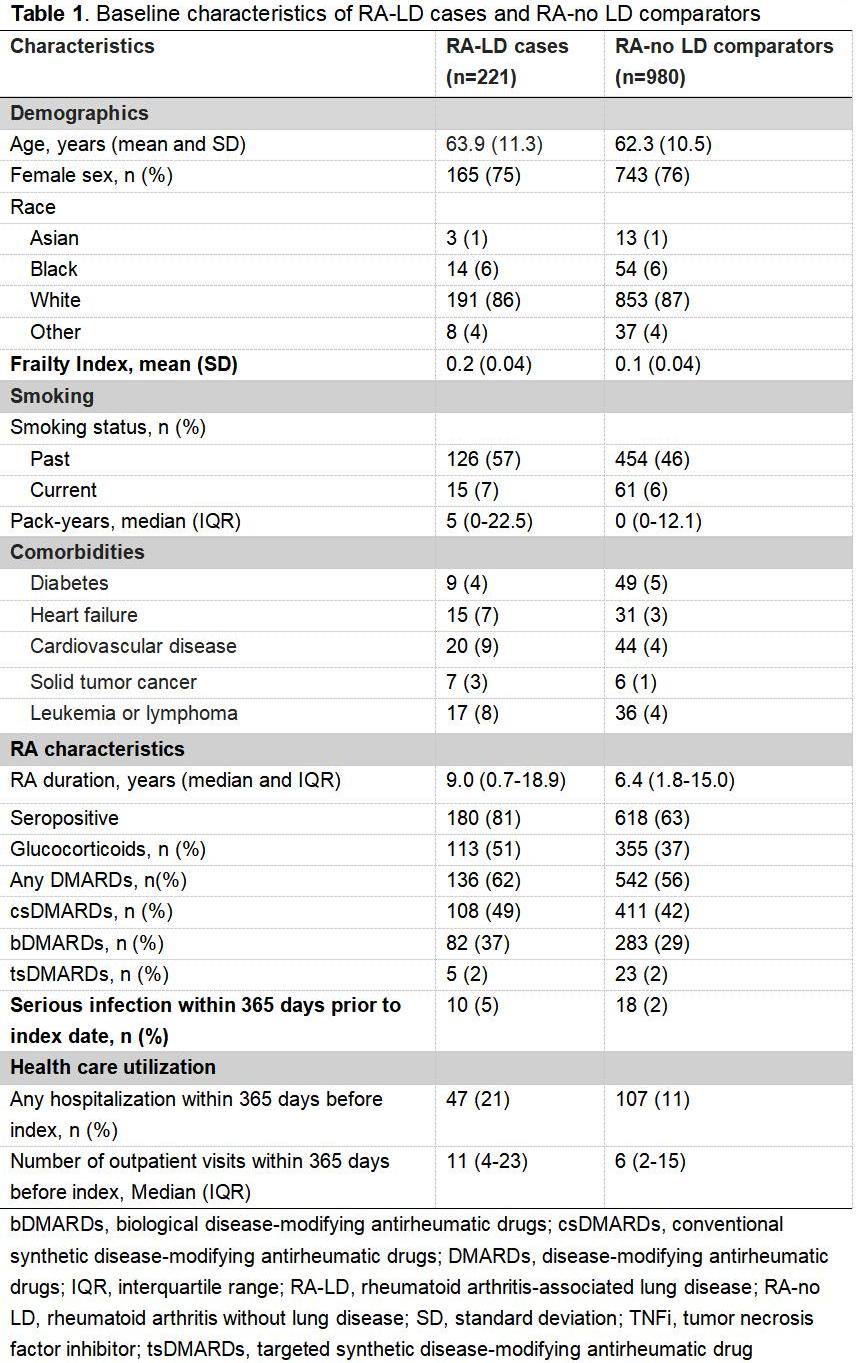
Methods: We conducted a retrospective matched cohort study of patients enrolled in the biobank of a large U.S. health care system, comparing RA-LD cases to RA comparators without lung disease (RA-no LD), matched by calendar date, age, sex, and RA duration at the index date. The index date was defined as the later date of the RA or ILD/BR diagnosis for RA-LD cases, and the matched date for RA-no LD comparators. Patients with RA met the 2010 ACR/EULAR classification criteria. RA-LD cases were verified by medical record review and chest imaging for clinically-apparent RA-ILD and/or RA-BR. The primary outcomes were overall and respiratory hospitalizations. Secondary outcomes included emergency department (ED) visits and intensive care unit (ICU) admissions. Incidence rates were calculated per 100 person-years. Incidence rate ratios (IRRs) with 95% confidence intervals (CI) were estimated using multivariable Poisson regression models, comparing RA-LD cases vs. RA-no LD comparators as well as for RA-ILD and RA-BR cases vs. RA-no LD comparators, with adjustment for the propensity score as a covariate.
Results: We analyzed 221 RA-LD cases (151 RA-ILD and 70 RA-BR) and 980 matched RA-no LD comparators (Table 1). RA-LD patients had higher rates of overall hospitalization (60% vs. 41%, p< 0.001) and respiratory hospitalization (23% vs. 6%, p< 0.001), along with higher proportions of ED visits (57% vs. 48%, p=0.02) and ICU admissions (36% vs. 20%, p< 0.001, Table 2). RA-LD patients had a shorter time from the index date to first hospitalization (median 922 vs. 1,217 days, p=0.01) compared to RA-no LD comparators. They also had a shorter time to first respiratory hospitalization (median 1,588 vs. 2,253 days, p=0.009), including RA-ILD (median 1,707 vs. 2,253 days, p=0.03) and RA-BR (median 1,436 vs. 2,253 days, p=0.04). RA-LD, including RA-ILD and particularly RA-BR, had higher risks of overall hospitalization (adjusted IRR 1.73, 95%CI 1.57-1.91) and respiratory hospitalization (adjusted IRR 5.13, 95%CI 3.80-6.94, Table 3). RA-ILD was associated with an increased risk of ICU admissions (adjusted IRR 1.99, 95%CI 1.81-2.18).
Conclusion: RA-LD was associated with higher risks of overall hospitalization, respiratory hospitalization, and ICU admissions than RA-no LD comparators. RA-BR had a similarly elevated hospitalization risk as RA-ILD, illustrating an unreported unmet need in this population. These findings highlight the need for targeted strategies to prevent and manage acute care utilization in RA patients with lung involvement.
To cite this abstract in AMA style:
ZHANG Q, Qi Y, Wang X, McDermott G, Chang S, Getachew L, Chaballa M, Khaychuk V, Paudel M, Liao K, Sparks J. Risk of hospitalization in patients with rheumatoid arthritis-associated interstitial lung disease or bronchiectasis: A matched cohort study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/risk-of-hospitalization-in-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease-or-bronchiectasis-a-matched-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-hospitalization-in-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease-or-bronchiectasis-a-matched-cohort-study/

.jpg)
.jpg)