Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Childhood chronic anterior uveitis (CAU) can be idiopathic (iCAU) or associated with Juvenile Idiopathic Arthritis (JIA-U). Ocular complications occur in 50% of affected children. Several cytokines, chemokines and S100 proteins have been associated with a diagnosis of CAU in children with JIA. Tear fluid analysis has emerged as a highly promising tool to study biomarkers. We aim to further investigate previously reported diagnostic biomarkers in tear fluid of children with JIA-U and their association with CAU activity, ocular complications and duration of CAU.
Methods: For this cross-sectional study, we collected tear samples from both eyes by Schirmer strips in children ≥5 years old diagnosed with oligo- or polyarticular RF negative JIA-U and iCAU. CAU activity was defined by Standardization of Uveitis Nomenclature criteria where anterior chamber (AC) cell grade 0 (< 1 cell/high power field) was inactive, and grades ≥0.5+ were considered active. For active CAU, we only included children with bilateral active CAU (excluded those with a contralateral inactive eye). Levels of S100A8, A9, and A12 were measured by ELISA, and IL-18, IL-8, IP-10, MCP-1, RANTES, and sICAM-1 by Luminex assays. Logistic regression and correlation analysis were used for statistical analysis and p-value < 0.05 are deemed significant. Biomarker levels were compared by: 1) CAU activity: active vs inactive CAU, then stratified by CAU type; 2) CAU complications: present vs. absent (e.g. cataract, glaucoma, synechiae, cystoid macular edema, band keratopathy); and 3) correlation between biomarkers level and duration of CAU in years.
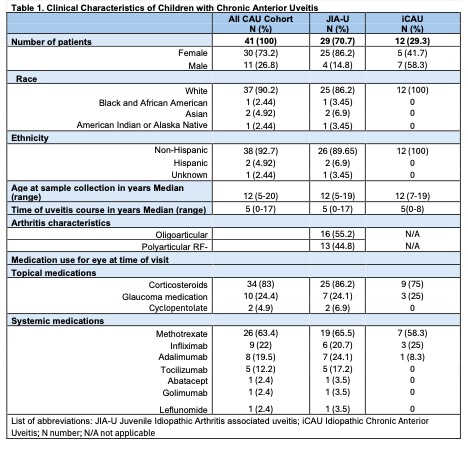
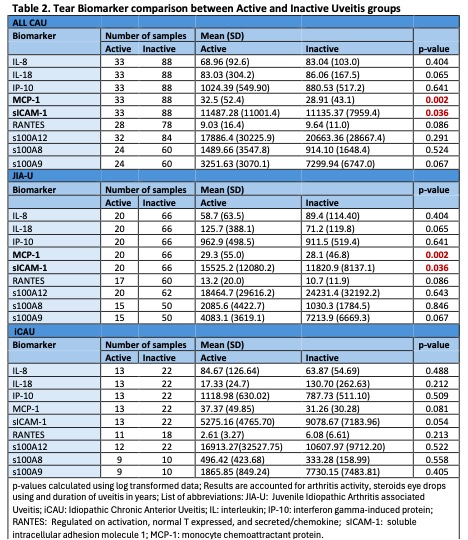
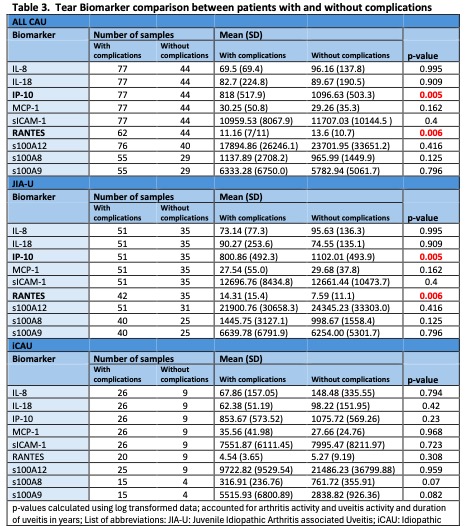
Results: Forty-one children (29 JIA-U; 12 iCAU) with CAU contributed 121 tear samples (86 JIA-U; 35 iCAU). Demographic and clinical information are described in Table 1. We observed an increased level of sICAM-1 (p=0.036) and MCP-1 (p=0.002) in children with active CAU compared to inactive CAU (Table 2). Results were similar when we restricted analysis to those with JIA-U only. Patients with ocular complications had significantly decreased levels of IP-10 (p=0.005) and RANTES (p=0.006) (Table 3). There was a positive correlation of longer CAU disease duration with levels of sICAM (p< 0.001) and s100A12 (p=0.012).
Conclusion: We identified potential tear-based biomarkers that are associated with CAU activity and ocular complications. We confirmed our previous findings in a larger cohort that sICAM-1, S100A12 and MCP-1 may reflect changes in ocular inflammation. Further, we newly show that IP-10 and RANTES may be associated with ocular damage. Investigations in larger cohorts of children with CAU are required to establish connections between tear-based biomarkers and processes in the eye such as CAU chronicity and damage, systemic inflammation and medication use.
To cite this abstract in AMA style:
Pavlenko M, Maccora I, Altaye M, brunner h, Duell A, Quinlan-Waters M, Sproles A, Thornton S, Miraldi Utz V, Angeles-Han s. Tear Biomarkers for Monitoring Disease Activity and Progression of Noninfectious Chronic Anterior Uveitis in Children [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/tear-biomarkers-for-monitoring-disease-activity-and-progression-of-noninfectious-chronic-anterior-uveitis-in-children/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tear-biomarkers-for-monitoring-disease-activity-and-progression-of-noninfectious-chronic-anterior-uveitis-in-children/