Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose:
Uveitis is the inflammation of the eye, which is third leading cause of preventable blindness in the United States. Corticosteroids are the first line of management to suppress inflammatory response. Patients with recurrent uveitis have structural complications that need prolonged course of steroids, resulting in iatrogenic complications. These are the patients who will need long term steroid sparing immunosuppressive therapy. A collaborative Rheumatology-Ophthalmology team approach could improve management of uveitis patients requiring prolonged immunosuppressive therapy. Our aim was to increase the percentage of uveitis patients, at risk of vision loss who are evaluated by the rheumatology team for initiation of steroid sparing therapy, these are patients with uveitis on topical steroid therapy for more than 6 months or oral steroid therapy for more than 2 months or patients with structural complications.
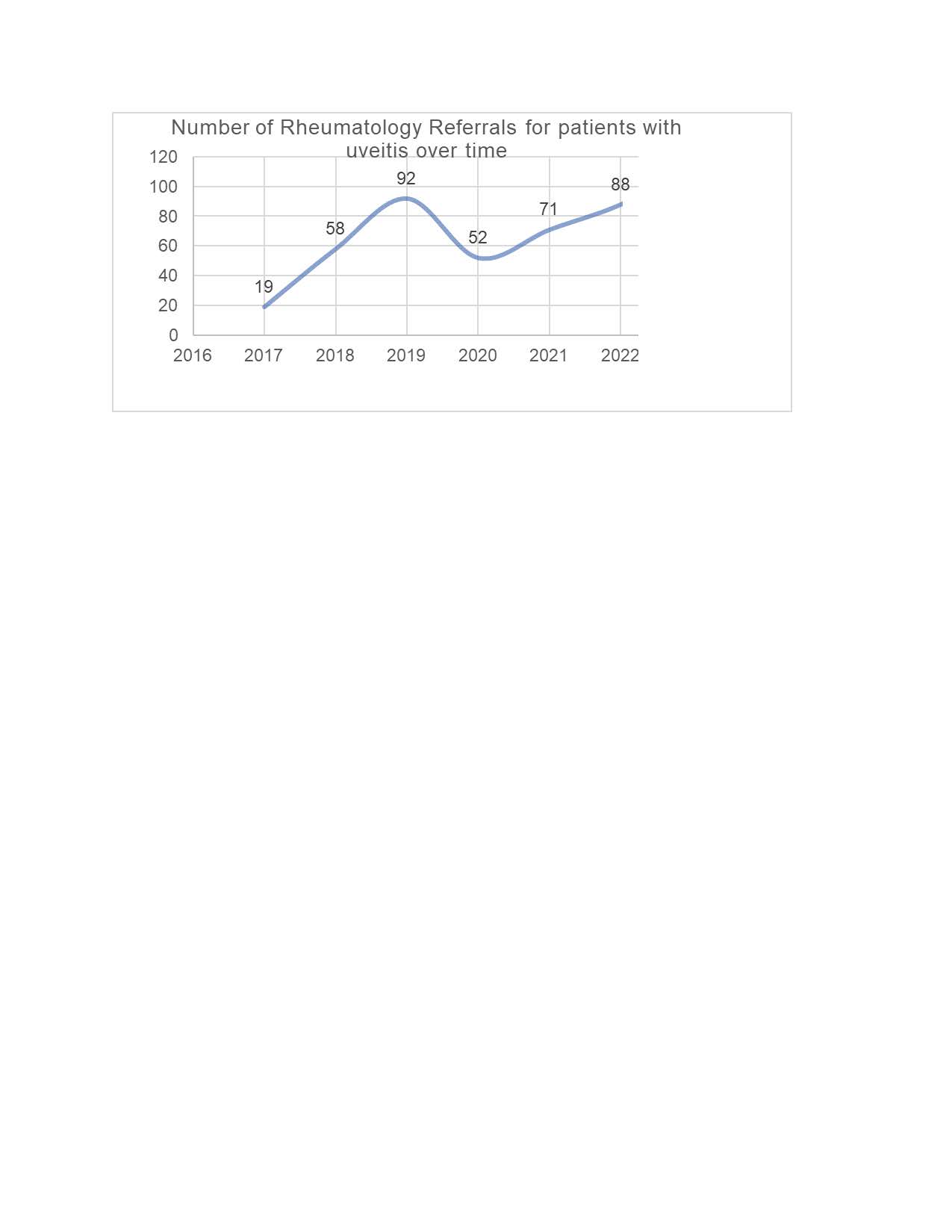
Methods: After the IRB approval, electronic medical records were queried (January 2017 – December 2023), to assess the baseline data we identified 2684 patients with uveitis, 41 experienced blindness and 501 patients had a referral to rheumatology. Of the 501 patients only 204 (41%) had a rheumatology appointment scheduled appointment (Figure 1). We queried the physicians, secretaries, patient scheduling staff and uveitis patients, to identify the barriers for timely scheduling rheumatology appointments. We utilized Quality Improvement (QI) tool, process map to outline the current uveitis patient scheduling practice at the Rheumatology clinic. To assess the progress of the QI intervention, we had uveitis patients who received referral documentation as the process measure and number of uveitis patients scheduled for the rheumatology appointment as the outcome measure.
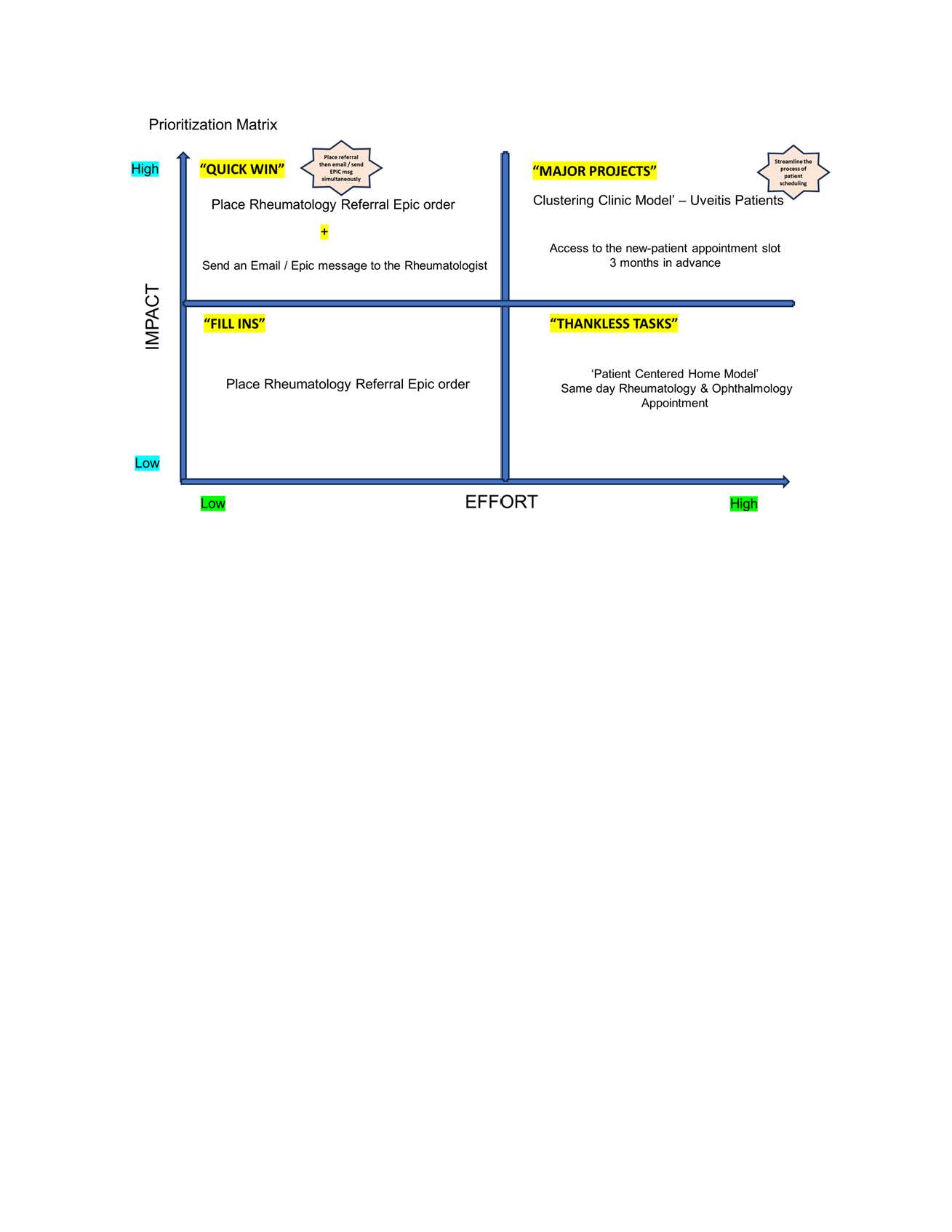
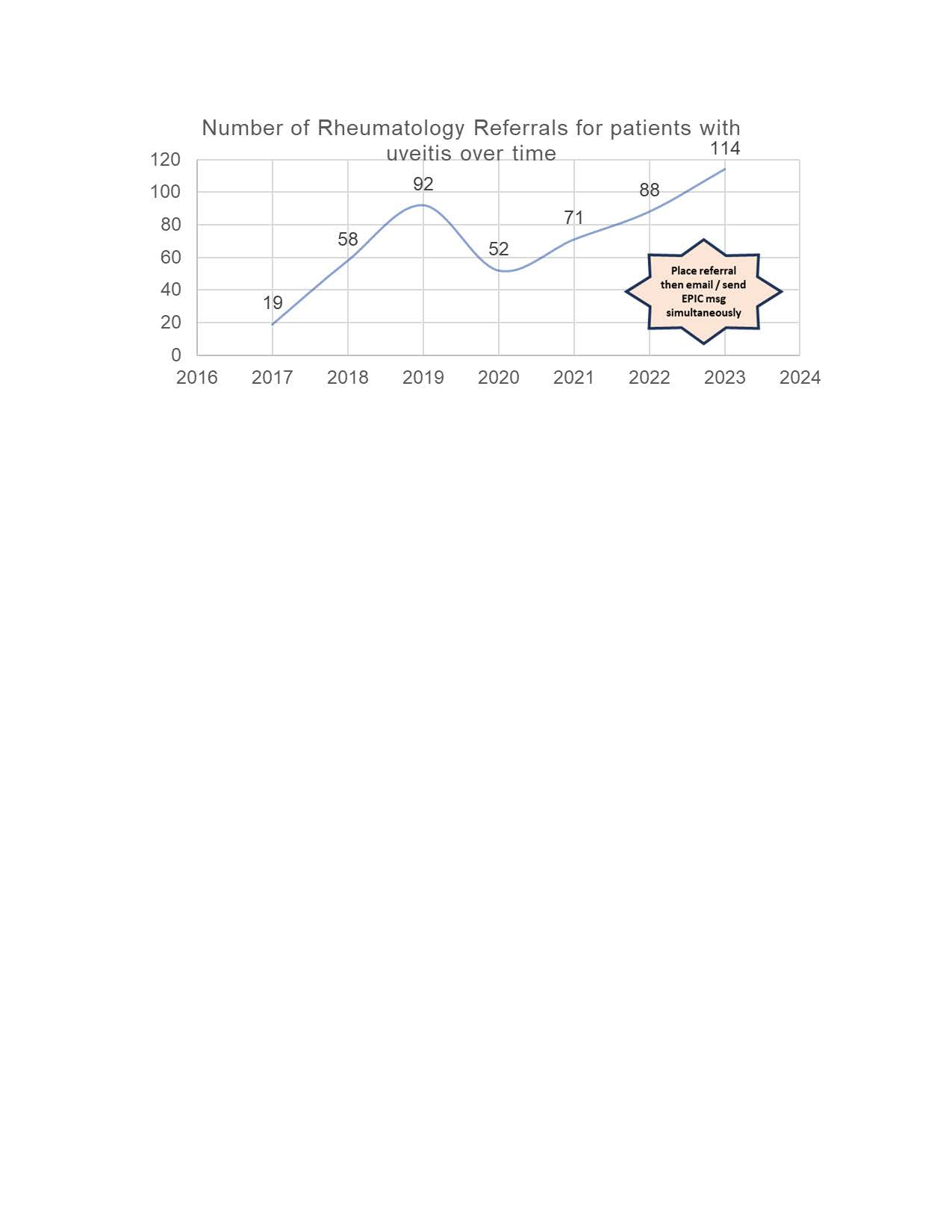
Results: We utilized prioritization matrix to plan the interventions (Figure 2). As the first intervention, plan-do-study-act (PDSA-1) cycle, we identified the ophthalmologist who treat uveitis patients and discussed with them to place referral electronic medical record (EMR) epic order and simultaneously email the rheumatologist, that increased the number of rheumatology referrals to 114 (Figure 3). To accommodate these increased referrals in the rheumatology clinic, we adapted clustering clinic model as PDSA cycle 2 by identifying the rheumatologist who treat uveitis patients with steroid sparing therapy and schedule the uveitis patients on a particular day week, to avoid over booking and streamline the clinic workflow.
Conclusion: We identified potential barriers to, uveitis patients getting timely rheumatology appointments. Our QI improvement results demonstrated that a collaborative Rheumatology-Ophthalmology team approach could improve timely scheduling rheumatology appointments for uveitis patients who require steroid sparing therapy. This initiative can be replicated on a larger scale to improve clinical care in patients requiring steroid sparing therapy.
To cite this abstract in AMA style:
Ayesha B, Castiblanco C, Tagoe C, Baron S, Rikin S. Timely Initiation of Steroid Sparing Therapy in Uveitis Patients – a Quality Improvement Initiative [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/timely-initiation-of-steroid-sparing-therapy-in-uveitis-patients-a-quality-improvement-initiative/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/timely-initiation-of-steroid-sparing-therapy-in-uveitis-patients-a-quality-improvement-initiative/