Session Information
Date: Monday, November 18, 2024
Title: Systemic Sclerosis & Related Disorders – Basic Science Poster II
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Cells of the monocyte-macrophages (Mφ) are key players in the pathogenesis of systemic sclerosis (SSc), contributing to inflammation and fibrosis. To advance beyond the simplified dichotomy of M1 vs. M2 often used in vitro, our study aims to explore the heterogeneity of monocytes and Mφ in SSc. We employed scRNA sequencing techniques to analyse these cells in blister fluid, and validated by AKOYA multiplex staining in situ, enabling us to precisely assess the population complexity and functional states of these cells. Furthermore, we employ an in vitro disease model that closely mimics SSc conditions, allowing us to replicate key disease features.
Methods:
Suction blister fluid was obtained from the lesional tissue of forearm skin of SSc patients (n=6) and healthy volunteers skin (n=4), and then profiled by 10X RNAseq. Downstream analysis was performed using standard Seurat pipeline, GSEA and RNA velocity. Monocyte and Mφ spatial localization was investigated using AKOYA multiplex histochemistry for 10 antibody probes designed to identify activated Mφ (CD206 and CD163) and adjacent vascular (SMA, CD31), stromal (FSP1, Vimentin, and Pan Cytokeratin) and immune populations (CD3e and CD8). SSc activation of blood monocyte-derived Mφ was investigated using 5% autologous patient plasma, isolated IgG from anti-topoisomerase (ATA) positive plasma, and ATA specific Ig-immunocomplexes.
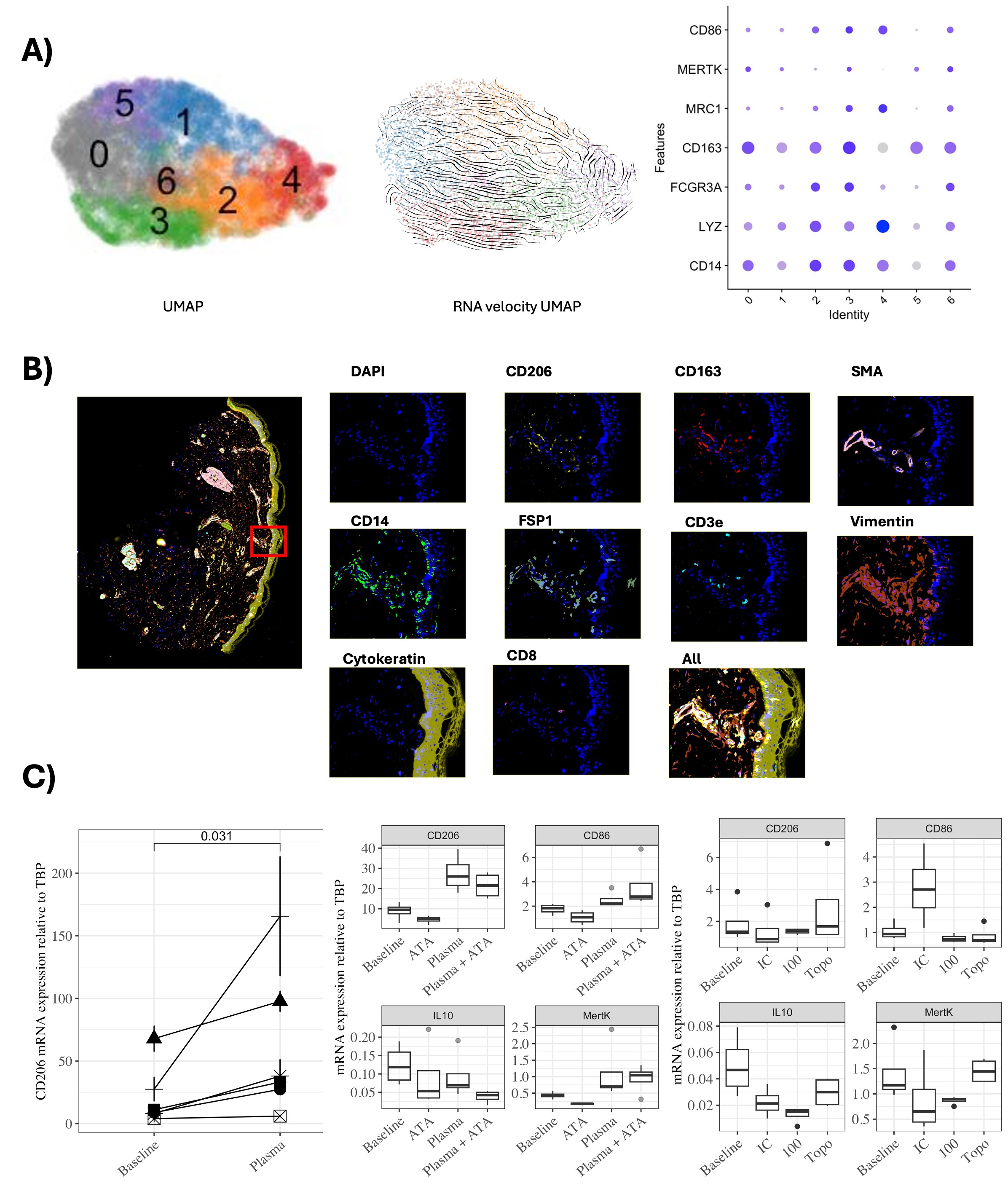
Results: Seven were monocyte/macrophage populations, including two specific monocyte populations and five distinct macrophage populations were identified standard Seurat pipeline and common monocytes and Mφ markers including LYZ, CD14, FCGR3A, CD163 and MRC1. RNA velocity analysis suggested a differentiation pathway from monocytes to macrophages (Mφ), with FCGR3A+ monocytes in Cluster 2 progressing towards macrophage subsets expressing ZEB2, UTR, and SLC9A9 in Cluster 3, or towards CSTB+ and CCL2high Mφ in Clusters 6 and 0 (Figure 1A). Additionally, a transition from NME1dim in Cluster 1 to NME1high in Cluster 5, and subsequently to CCL2+ Mφ in Cluster 0, supports the notion of macrophage plasticity within the blister fluid environment. In-situ localisation showed CD206+/CD163+ double-positive Mφ near blood vessels in the skin of SSc patients) (Figure 1B). In vitro, monocyte-derived populations exhibited increased CD206(p=0.0011), CD86 (p= 0.0479), and MERTK (p=0.0013) expression when stimulated with autologous plasma. The addition of anti-topoisomerase antibodies (ATA) to plasma or ATA immunocomplex (IC) increased CD86 expression (p=0.0320 and p=0.0076), suggesting an induction of M2b polarisation (Figure 1C) similar to cluster 3 found in transcriptomic analysis.
Conclusion: Our study using blister fluid reveals novel and distinct monocyte and macrophage subsets in blister fluid. These populations are highly plastic and include tissue resident Mφ and monocyte-derived differentiated into Mφ expressing CD206 (MRC1) and CD163. The localisation of monocyte derived Mφ adjacent to blood vessels, is consistent with monocyte transmigration into the tissue. In vitro stimulation by plasma or ICs increased activation markers indicating monocytes might be primed in the blood and further differentiate in the tissue.
A) UMAP shows different monocytes and Mφ populations, RNA velocity UMAP indicates monocyte to Mφ differentiation and Dotplot shows expression of activation markers. B) Representative multiplex immunohistochemistry staining showing macrophages near blood vessels. C) In vitro experiments showing plasma induction of CD206, and the effect of plasma and immunocomplexes in MDMφ activation markers (CD206, CD86, IL_10 and MERTK).
To cite this abstract in AMA style:
Lopez Garces S, Searle T, Zhang S, Lopez H, Elhussin I, Yates C, Abraham D, Denton C, Ahmed Abdi B, Stratton R. Understanding Monocyte Derived Macrophages in the Skin of SSc Patients Through Single Cell Analysis of Blister Fluid Immune Cell Populations [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/understanding-monocyte-derived-macrophages-in-the-skin-of-ssc-patients-through-single-cell-analysis-of-blister-fluid-immune-cell-populations/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/understanding-monocyte-derived-macrophages-in-the-skin-of-ssc-patients-through-single-cell-analysis-of-blister-fluid-immune-cell-populations/