Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Ambulatory care sensitive conditions (ACSCs) are conditions where appropriate access to ambulatory care can reduce hospitalizations. People with rheumatoid arthritis (RA) are at higher risk for ACSC hospitalizations due to consequences of systemic inflammation and insufficient management of the condition in ambulatory practice. This project aims to estimate rates of avoidable hospitalizations by persons with RA relative to the general population.
Methods: We conducted a retrospective cohort study in Alberta, Canada, a province of ~4.6M with universal health coverage, of individuals meeting a validated case definition for RA based on ICD codes in years 2002-2023. Controls were identified by matching age, sex, and date of diagnosis. There was a 5-year washout period to identify incident RA cases. We identified ACSCs using established ICD codes from the Canadian Institute for Health Information (including grand mal seizures, chronic lower respiratory diseases, asthma, diabetes, heart failure and pulmonary edema, hypertension, and angina). Incidence rate ratios (IRR) up to 5 years from the date of diagnosis were calculated using a multivariable regression model adjusting for age, sex, and location of residence. A Cox proportional hazards model (p < 0.05) was used to identify predictors of avoidable hospitalizations, including sex, age at admission, location of residence, attachment to a family physician or rheumatologist, exposure to corticosteroid and disease-modifying anti-rheumatic drugs (DMARDs), presence of comorbidities, and whether these comorbidities are ACSCs.
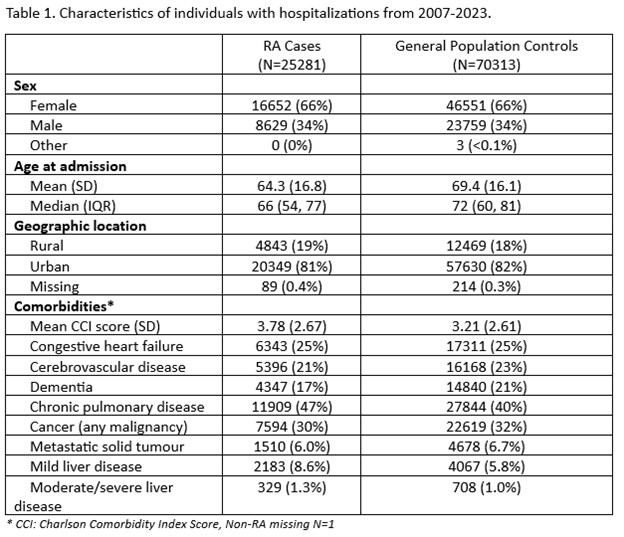
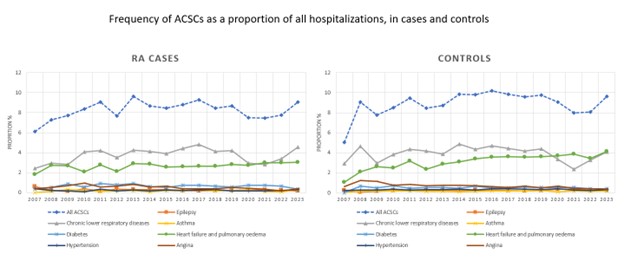
Results: From a prevalent RA cohort composed of 52,596 individuals and 210,384 controls, there were 25,281 cases and 70,313 controls with hospitalizations during the study period (Table 1). The number of hospitalizations was 83,811 in cases and 190,304 in controls, where 8.3% and 9.1% were for all ACSCs combined, respectively. Among cases, the highest frequency of ACSC hospitalizations was for chronic lower respiratory diseases at 3.8% (3202/83811) (Figure 1).
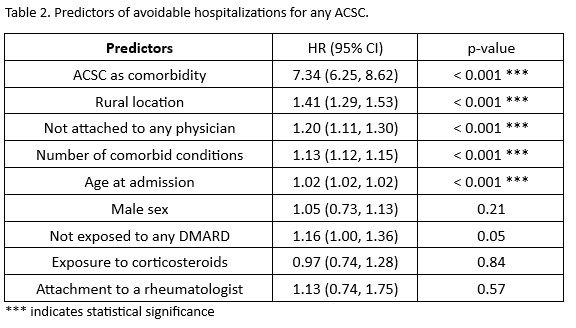
Cases had 1.12 times the risk of hospitalization for heart failure and pulmonary edema compared to those without RA (IRR 1.12, 95% 1.01, 1.25). Significant predictors of ACSC hospitalizations for RA cases were increasing age, not having seen a physician at any point since diagnosis, being from a rural location, and having comorbid conditions, especially if the comorbid condition is an ACSC (HR 7.34, 95% CI 6.25, 8.62) (Table 2).
Conclusion: Persons with RA are at a higher risk of avoidable hospitalizations in the first 5 years after diagnosis compared to those without RA. Improved ambulatory care access and quality, inclusive of primary care and subspecialty care, is needed to prevent unnecessary hospitalizations and reduce burden on the acute care system.
To cite this abstract in AMA style:
Contreras D, Barber C, Avina-Zubieta J, Quan H, Lee S, King J, Barnabe C. Avoidable Hospitalizations by Persons with Rheumatoid Arthritis: A Population-Based Study Using Administrative Data [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/avoidable-hospitalizations-by-persons-with-rheumatoid-arthritis-a-population-based-study-using-administrative-data/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/avoidable-hospitalizations-by-persons-with-rheumatoid-arthritis-a-population-based-study-using-administrative-data/