Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic sclerosis (SSc) is a rare systemic disease within the connective tissue disease (CTD) spectrum. It is characterized by microcirculatory abnormalities, skin and internal organ fibrosis, and presence of autoantibodies (Abs). Conventional autoantibodies include anti-topoisomerase I (Scl-70) Abs, anti-RNA polymerase III Abs and anti-centromere Abs. Other autoAbs, including anti U3-ribonucleoprotein, anti Th/To, anti-PM/Scl, anti-Ku, or anti-ribonucleoprotein U1 (anti-U1RNP) may also be present in SSc and are associated with distinct clinical features. Anti-U1RNP Abs are the hallmark of mixed connective tissue disease (MCTD) but are also found in other differentiated CTDs such as systemic lupus erythematosus (SLE). Anti-U1RNP Abs are present in 6-8% of SSc cases but their impact on the phenotype of these patients has been poorly characterized. Therefore, studies are essential to elucidate the impact of anti-U1RNP Abs on the clinical presentation and course of SSc patients. Taking advantage of the French SSc and MCTD national cohorts, we conducted a case-control study for this purpose.
Methods: We conducted a monocentric case-control, retrospective, observational, and longitudinal study using data from the French SSc and MCTD national cohort studies. For each patient with SSc and anti-U1RNP antibodies (SSc-RNP+), one patient with mixed connective tissue disease (MCTD) and 2 SSc patients without anti-U1RNP antibodies (SSc-RNP–) were matched for age, sex, and date of inclusion.
Results: Among the 1,184 SSc patients followed in our department, 64 (5.4%) had anti-U1RNP Abs and
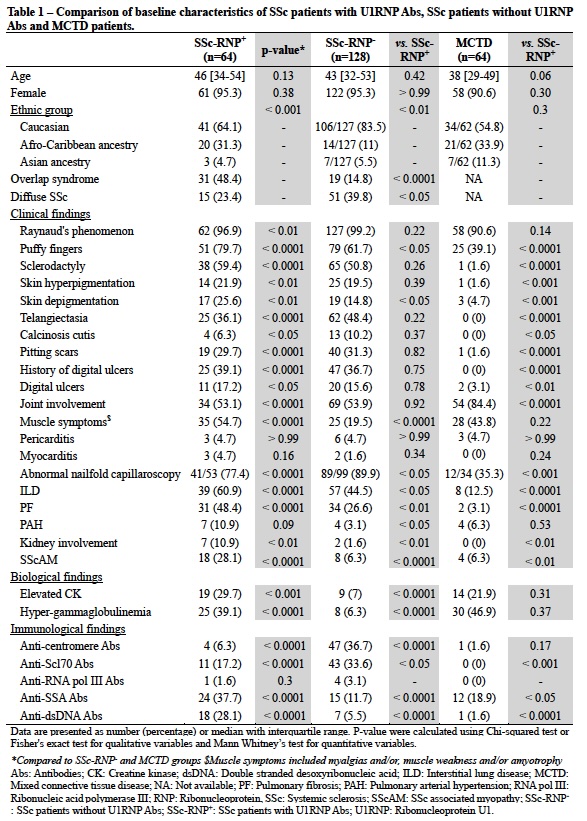
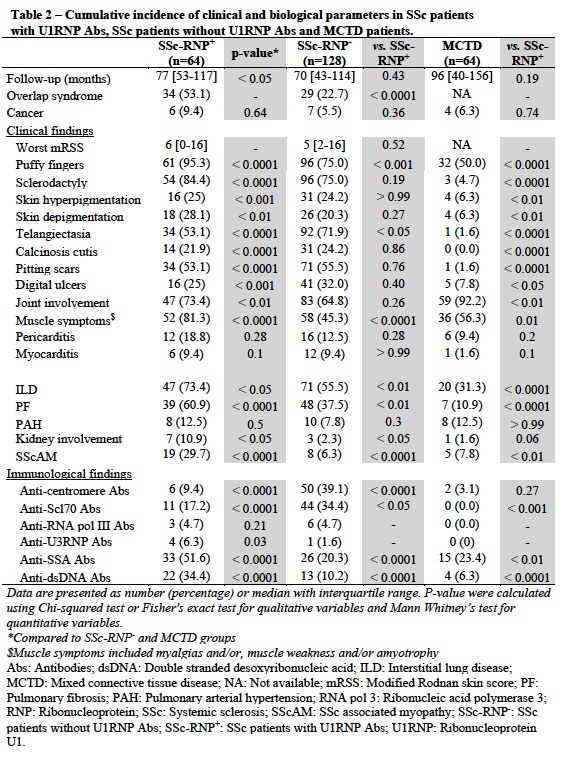
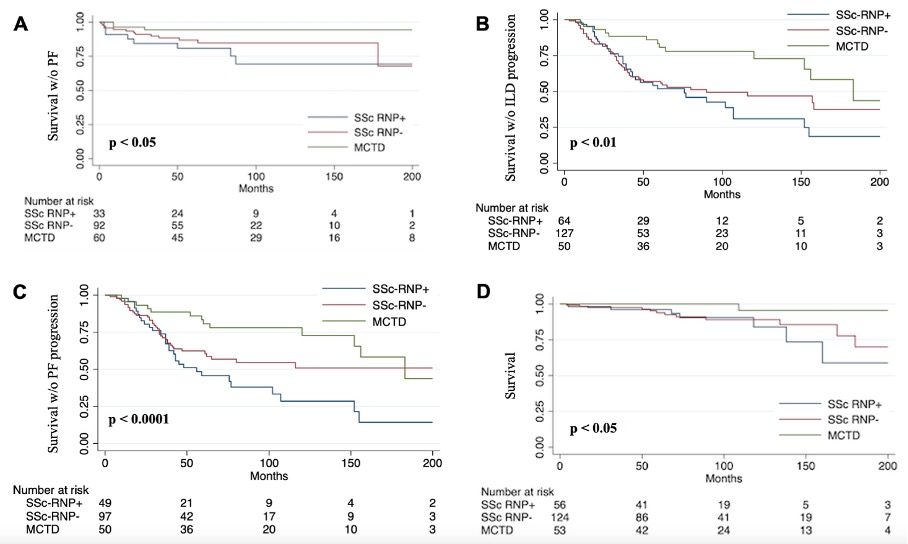
were compared to 128 SSc-RNP– and 64 MCTD patients. Compared to SSc-RNP–, SSc-RNP+ patients were more often of Afro-Caribbean origin (31.3% vs. 11%, p< 0.01), and more often had an overlap syndrome (53.1 % vs. 22.7%, p< 0.0001), overlapping with Sjögren’s syndrome (n=23, 35.9%) and/or SLE (n=19, 29.7%). At inclusion, ScS-RNP+ patients were more likely than ScS-RNP– or MCTD patients to have interstitial lung disease (ILD) (60.9% vs. 44.5% and 12.5%, p < 0. 0001), pulmonary fibrosis (PF) (48.4% vs. 26.6% and 3.1%, p < 0.0001), ScS-associated myopathy (SScAM) (28.1% vs. 6.3% and 6.3%, p < 0.01) and kidney involvement (p < 0.01) (Table 1). After a median follow-up of 77 [53-117] months, these differences persisted with significantly more frequent development of ILD (p < 0.05), PF (p < 0.0001), SScAM (p < 0.0001) or kidney involvement (p < 0.5) in ScS-RNP+ patients compared to ScS-RNP– or MCTD patients (Table 2). Over a 200-month follow-up period, SSc-RNP+ patients had worse survival without PF occurrence (p< 0.01) (Figure 1A), ILD or PF progression (p< 0.01 and p < 0.0001) (Figure 1B and C) and worse overall survival (p< 0.05) (Figure 1D).
Conclusion: In SSc patients, anti-U1RNP antibodies are associated with a higher incidence of overlap syndrome, a distinct clinical phenotype, and poorer survival compared to SSc-RNP– and MCTD patients. Our study suggests that SSc-RNP+ patients should be separated from MCTD patients and may constitute an enriched population for progressive lung disease.
Kaplan–Meier curves showing the 200-month probability of survival without pulmonary fibrosis (Panel A), without interstitial lung disease progression (Panel B), without pulmonary fibrosis progression (Panel C), and overall survival (Panel D) of SSc-RNP+ patients compared to those of SSc-RNP- and MCTD patients.
PF: pulmonary fibrosis; ILD: Interstitial lung disease; MCTD: Mixed connective tissue disease; SSc: Systemic sclerosis; SSc-RNP-: SSc patients without U1RNP antibodies; SSc-RNP+: SSc patients with U1RNP antibodies.
To cite this abstract in AMA style:
Chevalier K, Chassagnon G, LOUIS-LEONARD S, cohen P, Dunogue b, Régent A, Thoreau B, Mouthon L, Chaigne B. Anti-U1RNP Antibodies Are Associated with a Distinct Clinical Phenotype and a Worse Survival in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anti-u1rnp-antibodies-are-associated-with-a-distinct-clinical-phenotype-and-a-worse-survival-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-u1rnp-antibodies-are-associated-with-a-distinct-clinical-phenotype-and-a-worse-survival-in-patients-with-systemic-sclerosis/