Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Nailfold videocapillaroscopy (NVC) alterations have mostly been described in autoimmune inflammatory myopathies (AIM) classified using Bohan and Peter criteria. The aim of this study was to describe NVC abnormalities in AIM subsets using contemporary sero-clinico-pathological criteria and explore the utility of current NVC patterns in AIM.
Methods: We studied AIM subjects in the Canadian Inflammatory Myopathy Study (CIMS), an early onset cohort followed prospectively. NVC images were acquired using the DS MEDICA Videocap (X200 magnification). The nailfolds of the second, third, fourth and fifth fingers of both hands were photographed and scored by an experienced rheumatologist. Microhemorrhages, giant capillaries, ectasias and ramified capillaries were scored using a standardized semi-quantitative scale (0 = no, 1 = ≤33%, 2= 33–66%, and 3 = ≥66% abnormalities per linear millimeter). Capillary density was scored semi-quantitatively (0 if ≥7, 1 if 4–6, or 2 if ≤3 capillaries/mm) and quantitatively (mean number of capillaries/mm). Each NVC parameter, as well as giant-ramified capillaries, were scored as present or absent. Finally, NVC patterns (i.e., scleroderma, sleroderma-like, late scleroderma, non-specific, and normal) were assigned. NVC features and patterns were compared between AIM subsets.
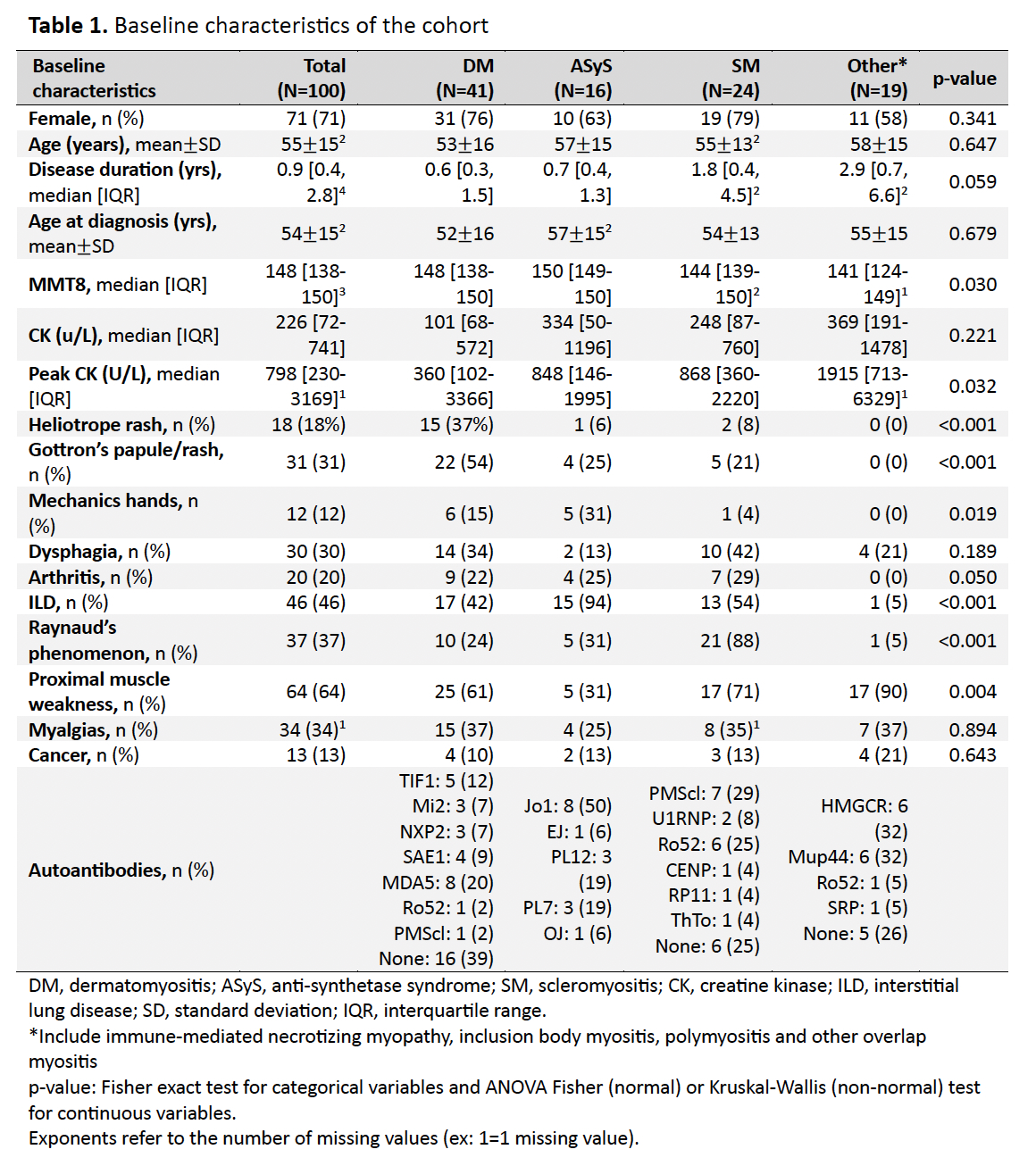
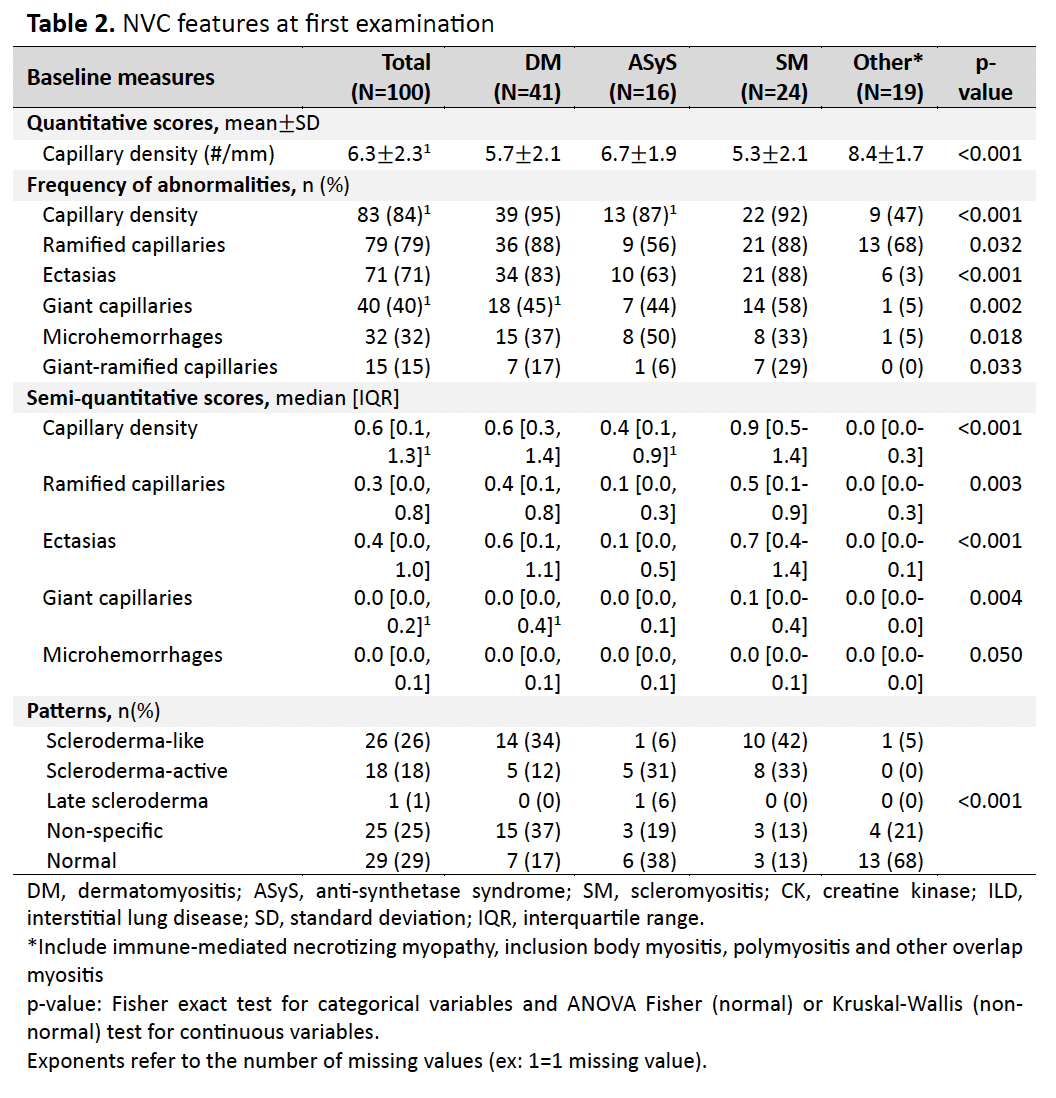
Results: We included 100 AIM subjects: 41 dermatomyositis (DM), 24 scleromyositis (SM), 16 anti-synthetase syndrome (ASyS), 7 immune-mediated necrotizing myopathy (IMNM), 8 inclusion body myositis (IBM), 3 polymyositis (PM) and 1 overlap myositis (Table 1). Of those, 71% were female, and median disease duration of 0.9 years. In the cohort, 45% of subjects had abnormal NVC, 25% non-specific NVC , and 29% normal NVC patterns. When NVC features were compared between AIM subsets (Table 2), DM and SM had the lowest capillary densities (5.7 capillaries/mm and 5.3 capillaries/mm, respectively, p< 0.001). NVC abnormalities were frequent in DM, ASyS and SM, although median semi-quantitative scores showed that abnormalities were found in less than 33% of capillaries studied. NVC patterns were not discriminant for DM, ASyS and SM, with scleroderma-like, scleroderma-active and non-specific patterns described in those 3 subsets. Apart from ramified capillaries, NVC abnormalities were infrequent in IMNM, IBM and PM.
Conclusion: In this cohort of AIM subjects classified using a sero-clinico-pathological approach, DM, ASyS and SM showed frequent NVC abnormalities, although no NVC pattern of abnormalities was associated with a particular subset demonstrating that current NVC pattern descriptions are not useful for AIM subsetting.
To cite this abstract in AMA style:
Cotton T, Leclair V, Berger C, Troyanov Y, Hudson m, Gyger G. Nailfold Videocapillaroscopy Abnormalities in Different Autoimmune Inflammatory Myopathy Subsets [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/nailfold-videocapillaroscopy-abnormalities-in-different-autoimmune-inflammatory-myopathy-subsets/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nailfold-videocapillaroscopy-abnormalities-in-different-autoimmune-inflammatory-myopathy-subsets/