Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoarthritis (OA) is an age-related joint disease that causes chronic pain and limited mobility. Patients mainly have access to therapies aimed at reducing inflammation and pain, mainly through the use of corticosteroids. Despite the societal and economic impact of OA, there’s a lack of treatments that act on the natural history of the disease, urging the exploration of novel strategies. Our team is focusing on intra-articular (IA) glucagon-like peptide-1 (GLP-1) analogs, which have anti-inflammatory and tissue-protective effects in addition to their antidiabetic properties. Here, we aimed to explore the analgesic, anti-inflammatory and protective effects of liraglutide (LIRA), a GLP-1 analogue, in an in vivo model of inflammatory OA in rats.
Methods: The effects of one IA injection of LIRA, dexamethasone (DEX) or vehicle on analgesia and knee joint structure were evaluated in a monoiodoacetate (MIA) rat model. Some animals received saline injection instead of MIA (sham animals). Allodynia was evaluated to assess pain behavior. Histologic analyses of synovial membrane (Krenn score) and cartilage (OARSI score for tibia and femur) were performed blindly by independent investigators, to evaluate synovial and cartilage structural changes. Krenn score (Krenn et al, 2006) is based on the scoring of the synovial membrane’s inner layer, resident cell density, and inflammatory infiltrate. OARSI score (Pritzker et al, 2006) is based on the depth (grade) and extent (stage) of lesions on the tibial plateau and femoral condyles.
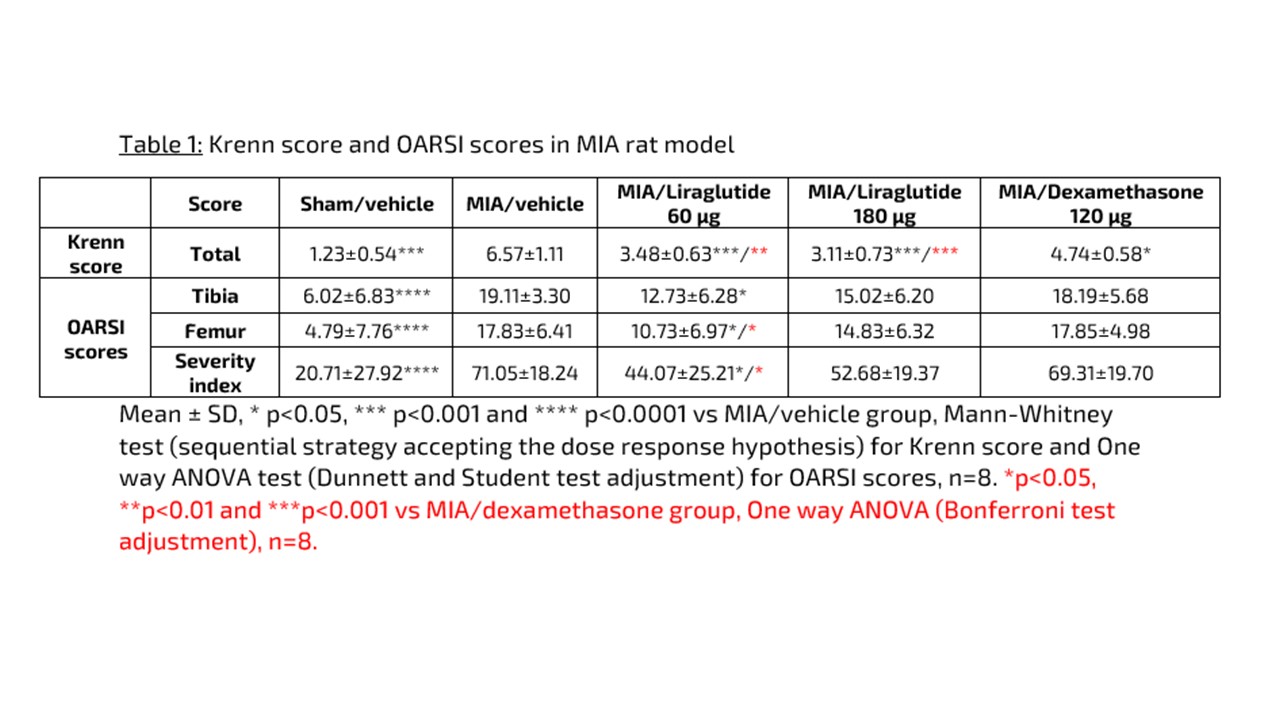
Results: IA injection of MIA induced a significant decrease in paw withdrawal threshold in vehicle animals compared to sham animals (p< 0.001). A single IA injection of LIRA or DEX induced a significant increase in paw withdrawal threshold compared to vehicle animals (p< 0.001 for the 3 groups on day 7, p< 0.01 for LIRA 60µg and p< 0.001 for LIRA 180µg and DEX on day 25). MIA injection induced a significant increased Krenn score compared to sham animals (p< 0.001). LIRA 60 and 180μg significantly reduced the MIA-induced Krenn score with a dose response (p< 0.001) compared to MIA/vehicle group. DEX slightly reduced the synovial score compared to MIA/vehicle group (p< 0.05). Moreover, data show a higher potential of LIRA to reduce the synovial score compared to the standard of care. LIRA 60µg significantly reduced the OARSI scores (p< 0.05) compared to MIA/vehicle group. Moreover, LIRA 60µg significantly reduced the femur score compared to DEX animals (p< 0.05). LIRA 180µg also tended to reduce the tibial and femoral scores compared to MIA/vehicle group. In comparison, DEX had no effect on the OARSI cartilage scores. When tibia and femur were considered, LIRA 60µg significantly reduced the global severity index compared to vehicle- or DEX treated animals (p< 0.05) (Table 1).
Conclusion: These results confirm that IA injection of LIRA effectively targets key aspects of OA, providing significant analgesic, anti-inflammatory, and joint structure protective effects. LIRA demonstrates greater potency compared to DEX in preserving synovial tissue and cartilage integrity. This underscores LIRA’s potential as a superior treatment option for OA, addressing both symptomatic relief and structural preservation.
To cite this abstract in AMA style:
Meurot C, Martin C, Vieubled M, Breton J, Toillon I, Rattenbach R, Berenbaum F. Beyond Pain and Inflammation: Intra-articular Liraglutide’s Comprehensive Benefits on Synovial Health and Cartilage in Osteoarthritis Compared to Dexamethasone [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/beyond-pain-and-inflammation-intra-articular-liraglutides-comprehensive-benefits-on-synovial-health-and-cartilage-in-osteoarthritis-compared-to-dexamethasone/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/beyond-pain-and-inflammation-intra-articular-liraglutides-comprehensive-benefits-on-synovial-health-and-cartilage-in-osteoarthritis-compared-to-dexamethasone/