Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Emergency departments (ED) become a location for non-urgent care when ambulatory care systems are not sufficient. We aim to describe contributing factors to the decision taken by persons with inflammatory arthritis (IA) to present to the ED, their experiences of ED care, and propose enhancements in ambulatory models of care to better support patients and improve system efficiency.
Methods: An invitation to complete an online survey was distributed by the health authority in October 2021 and March 2022 to a sample of individuals with an IA condition who had visited an ED within the previous year. Descriptive statistics were used to summarize quantitative data. Thematic analysis of free text responses was conducted to contextualize decision making and experiences of ED care, and generate system-level recommendations to reduce avoidable ED use.
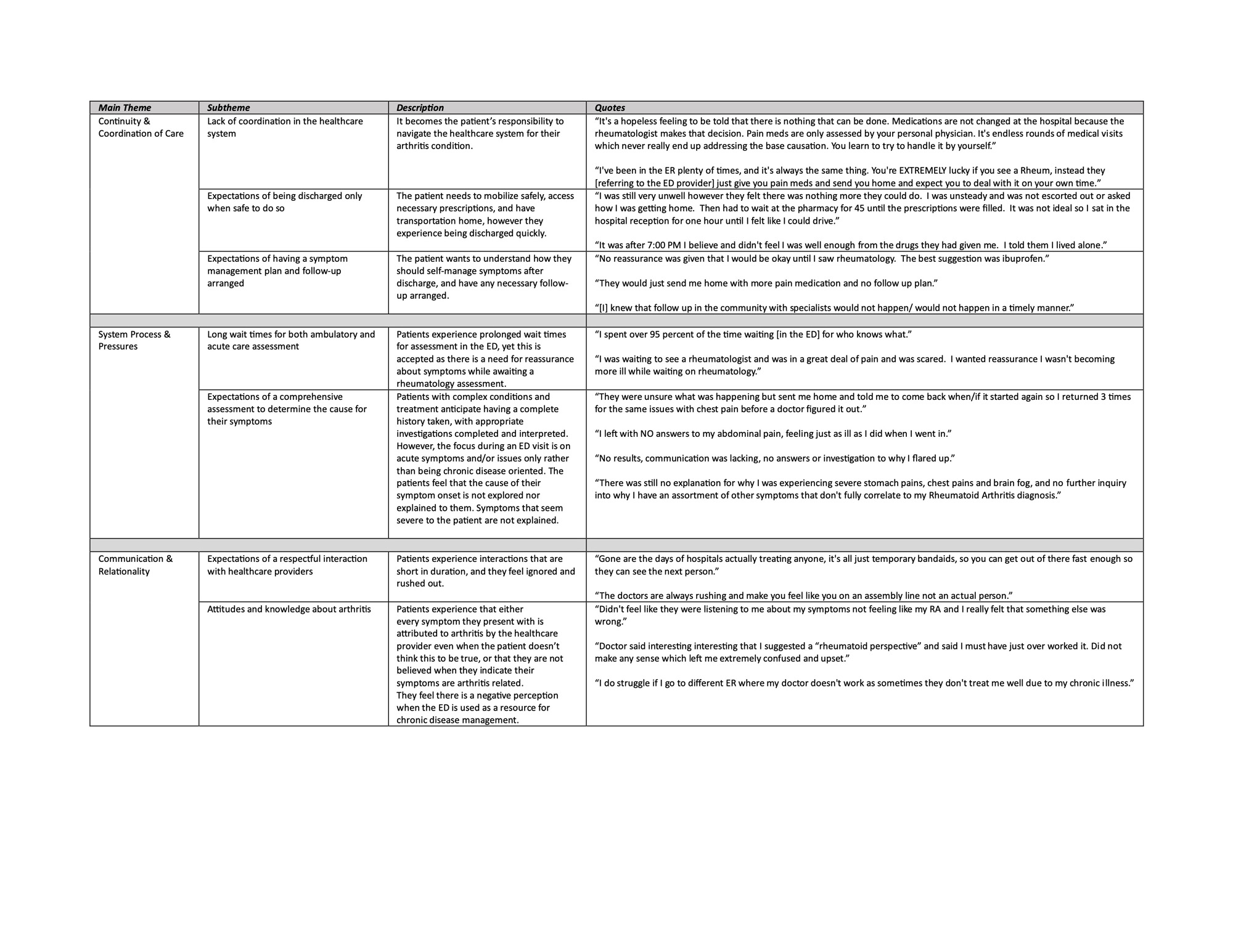
Results: 82 persons (48% RA, 12% PsA, 6% SpA, 34% Gout; 63% aged 16-55 years; 48% female; 50% urban residents) completed the survey. Over 1/3 (37%) of visits were for arthritis flare or other musculoskeletal symptoms, with other primary symptoms being chest pain (15%), injury (12%) and infection (11%). Of all visits, 28% of persons reported they proceeded directly to the ED, 32% made a return visit, and 36% were completed after accessing ambulatory care, primarily a primary care provider. For visits specific to arthritis flare or other musculoskeletal symptoms, 19% of patients proceeded directly to the ED as they could not access ambulatory care (after business hours, or call to provider not returned), 36% were a return visit of which 64% were for symptoms being unresolved or worsening and with 27% not being able to follow-up with their rheumatologist. For 39% they had accessed primary or specialty care for assessment and management first but then presented to the ED anyways. The rheumatology service was contacted by the ED provider in 9% of events of patients presenting with arthritis flare. Challenges in healthcare system coordination, system processes and pressures, and communication and relationality between IA patients and healthcare providers led to negative experiences of ED care (Table 1). After an ED visit patients had remaining concerns about not having been assessed comprehensively, and not having the cause of their symptoms being explained to them. They felt they were being discharged too soon, did not have a symptom management plan, and had the responsibility to coordinate multiple further assessments with different ambulatory providers. They perceived symptoms were not being appropriately attributed to their arthritis condition, Recommendations to reduce avoidable ED use include improving access to rheumatology care for both initial visits and urgent concerns, introducing initiatives for improved ambulatory care coordination and service delivery, resourcing EDs at appropriate levels to provide quality care, and to enhance provider education about arthritis condition assessment and management.
Conclusion: We present initial recommendations to develop systems and procedures to reduce the need for ED use by IA patients. Modifying current models of care may improve patient outcomes while simultaneously decreasing utilization and cost to the healthcare system.
To cite this abstract in AMA style:
Pianarosa E, Roach P, McLane P, Elliott M, Holroyd B, McQuitty S, Katz S, Russon N, Lin K, Barber C, Barnabe C. Identifying Inflammatory Arthritis Ambulatory Care Service Model Enhancements Needed to Reduce Avoidable Emergency Department Use [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/identifying-inflammatory-arthritis-ambulatory-care-service-model-enhancements-needed-to-reduce-avoidable-emergency-department-use/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identifying-inflammatory-arthritis-ambulatory-care-service-model-enhancements-needed-to-reduce-avoidable-emergency-department-use/