Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: There has been limited study of the risk of heart failure (HF) subtypes in RA at a population level, given the requirement for left ventricular ejection fraction (LVEF) from unstructured echocardiographic data to define HF with preserved (HFpEF) or reduced (HFrEF) ejection fraction. As the underlying pathophysiology differs, understanding the burden of HF subtypes in RA and whether advances in RA management have impacted their development is critical. Thus, we examined the risk and temporal trends of HFrEF and HFpEF in RA, leveraging LVEF values derived from natural language processing (NLP) in national Veteran’s Health Administration (VA) data.
Methods: We conducted a retrospective, matched cohort study of RA patients (≥2 RA ICD codes, rheumatologist diagnosis, and positive autoantibody or DMARD fill) matched up to 10 comparators (no RA ICD codes) on age, sex, and VA enrollment year. Patients with prevalent HF (≥1 ICD code prior to index) were excluded. Incident HF events were defined as a primary hospital discharge diagnosis or HF-related death, linking VA, Medicare, and National Death Index data. Echocardiogram-derived LVEF values were extracted from clinical notes using a validated NLP tool. HFrEF (EF < 50%) and HFpEF (EF ≥50%) were defined using the most proximate LVEF within 1 year prior to a HF event, or if missing, < 30 days following the event. We examined the association of RA with incident HFrEF and HFpEF separately in multivariable Cox regression models, stratified on matched pairs and censoring patients if they developed HF with no available LVEF, the alternative HF subtype, death, or reached end of study period (01/2020). Models were adjusted for demographics, smoking status, BMI, comorbidity burden, and healthcare utilization (number of hospitalizations in the year prior to index). Temporal trends were evaluated in an incident RA subcohort (no RA diagnostic codes or medication for >365 days following VA enrollment) by testing the interaction of RA status and sequential time periods in a linear manner, then stratifying analyses on RA diagnosis year (2000-2005, 2006-2011, 2012-2017).
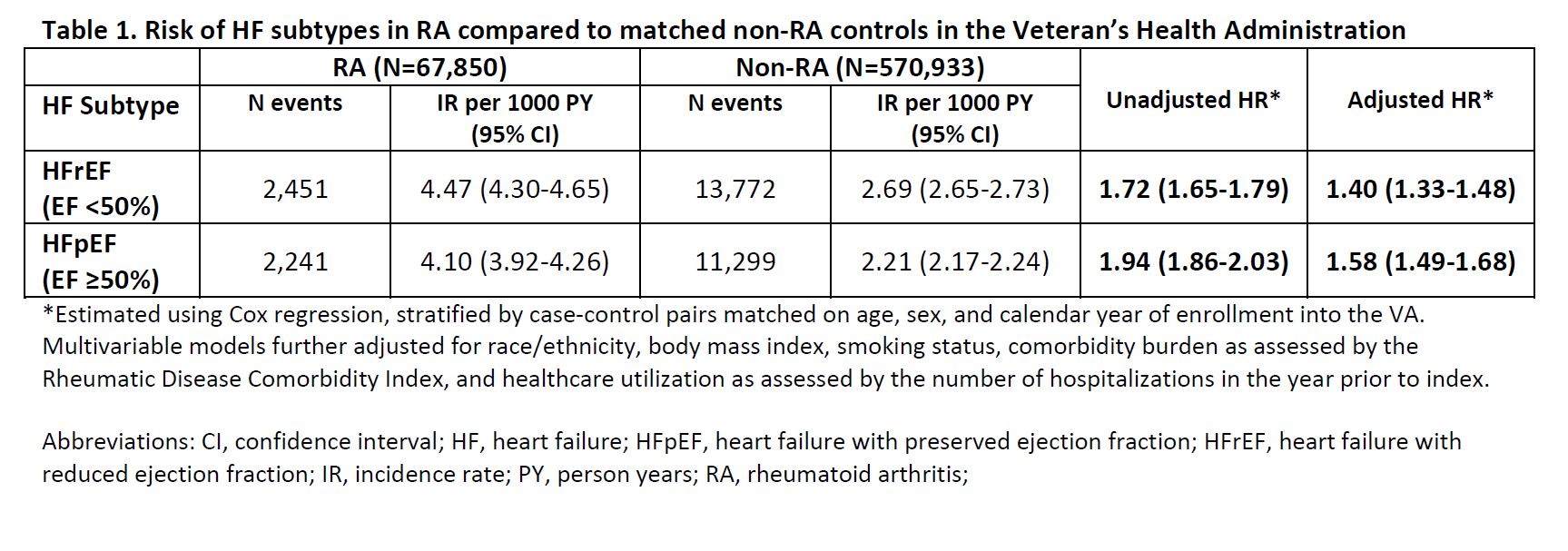
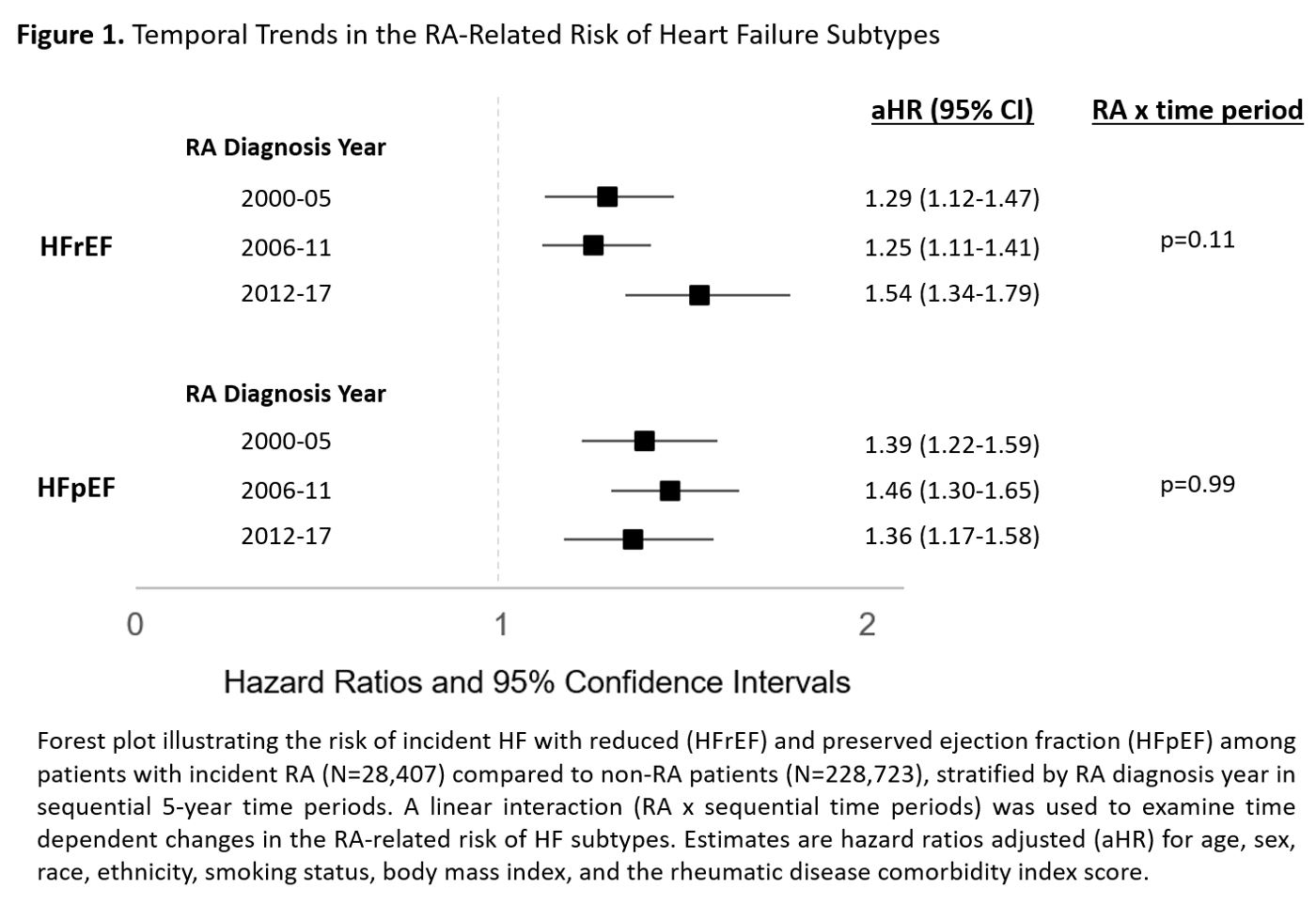
Results: We matched 67,850 RA patients (mean 62 years, 87% male) to 570,933 patients without RA. Over a mean follow up of 8.9 years (5,663,152 person-years), we observed 5,983 incident HF events in RA (10.9 per 1000 PY) vs. 40,283 events in non-RA (7.9 per 1000 PY) (Table 1). LVEF values were identified in 82% of RA vs. 68% of non-RA patients who developed incident HF. After multivariable adjustment, RA patients were at an increased risk of HFpEF (adjusted HR [aHR] 1.58, 95% CI 1.49-1.68) and HFrEF (aHR 1.40, 1.33-1.48). Among the incident RA subcohort (N=28,407 RA; 228,723 non-RA), we observed no improvement in the RA-related risk of HFpEF (range aHR 1.36-1.46) or HFrEF (range aHR 1.25-1.54) over time (Figure 1).
Conclusion: In this large, matched cohort study, patients with RA experienced a 58% increased risk of HFpEF compared to a 40% increased risk of HFrEF. No significant change was observed in the RA-related risk of either HF subtype over time. These findings suggest that RA-related HF risk persists despite major RA treatment advances and highlights the need to elucidate the factors contributing to the ongoing heightened risk of HF in RA.
To cite this abstract in AMA style:
Johnson T, Yang Y, Roul P, Baker J, Sauer B, Cannon G, Mikuls T, England B. Risk and Temporal Trends of Heart Failure Subtypes in Rheumatoid Arthritis: A National Veterans Affairs Matched Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/risk-and-temporal-trends-of-heart-failure-subtypes-in-rheumatoid-arthritis-a-national-veterans-affairs-matched-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-and-temporal-trends-of-heart-failure-subtypes-in-rheumatoid-arthritis-a-national-veterans-affairs-matched-cohort-study/