Session Information
Date: Saturday, November 6, 2021
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Cardiovascular Pulmonary Disease (0268–0295)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Cardiovascular disease (CVD) is the leading cause of mortality in rheumatoid arthritis (RA), but traditional CVD risk factors may not accurately characterize risk. For example, RA patients with a high body mass index (BMI) are not always observed to have higher long-term risks of obesity-related complications, perhaps as the result of long-term pathologic weight loss. Self-report of weight loss may thus serve as a helpful tool in risk-stratification by identifying individuals with adverse metabolic health. In this study, we evaluated the relationship between weight loss since age 30 and CVD along with factors associated with weight loss in patients with RA.
Methods: We studied RA patients ( >40 years old, without prior heart disease) enrolled in the FORWARD registry from 1998 to 2021. Weight change from reported weight at age 30 to enrollment was categorized as >10% weight loss, 5-10% weight loss, stable weight, and ≥5% weight gain (reference, due to being the expected change in lifespan). The primary outcome was a composite of nonfatal and fatal CVD since enrollment identified using ICD-9/10 codes (myocardial infarction [MI], stroke, and heart failure [HF]) and validated using hospital/death records. Secondary outcomes were individual CVD events. Multivariable Cox proportional hazards models were used to evaluate associations for weight changes adjusting for confounding variables (age, sex, race, enrollment BMI, year, RA duration, smoking, methotrexate, prednisone, biologic DMARD use). Models were further adjusted for factors that might be influenced by metabolic disturbance and contribute to CVD including the Rheumatic Disease Comorbidity Index (RDCI), Health Assessment Questionnaire Disability Index (HAQ) score, pain score, severity score, diabetes, hypertension, and lung disease.
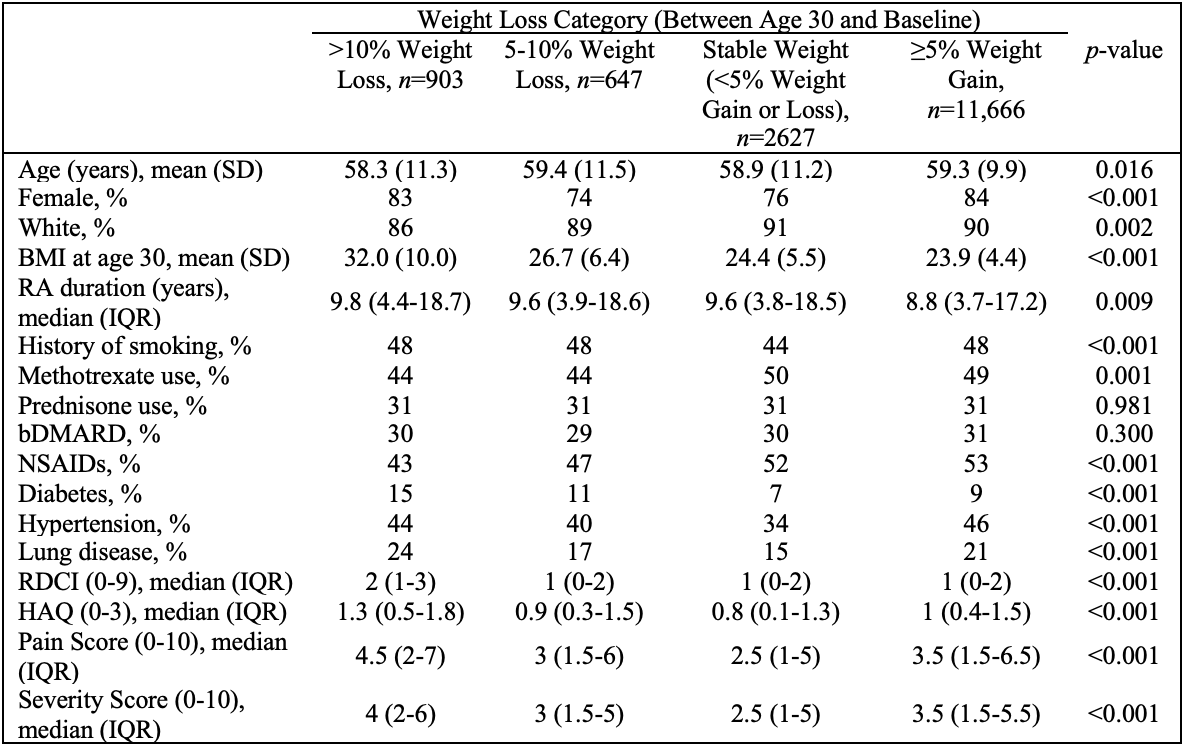
Results: Among 15,843 participants, 6% had >10% weight loss, 4% had 5-10% weight loss, 17% had a stable weight, and 74% had ≥5% weight gain since age 30. Participant characteristics differed substantially by weight change category (Table 1). There were 579 CVD incidents over 109,211 person-years of follow-up. Weight loss of >10% since age 30 was associated with 50% greater CVD risk independent of baseline BMI category and other baseline characteristics (HR 1.50, 95% CI 1.03-2.17). Weight loss ( >10%) was also associated with a 2-fold increase in fatal CVD risk (HR 2.0, 95% CI 1.27-3.16) (Figure 1) and increased MI (HR 1.57, 95% CI 0.88-2.80) and HF risks (HR 1.58, 95% CI 0.99-2.52), although the latter two did not reach statistical significance. Fully adjusted models that considered metabolic diseases, total comorbidity, disability, and symptoms demonstrated no significant association between weight loss and CVD events (HR: 1.23, 95% CI 0.83-1.82) (Table 2).
Conclusion: Long-term weight loss of >10% body weight is associated with increased CVD risk in RA independent of baseline BMI. The effect is largely explained by a higher prevalence of metabolic risk factors, comorbidity, and disability at enrollment, suggesting that the risk of weight loss in patients with RA is likely explained by worse metabolic health. Historical weight loss may serve as a marker of adverse metabolic health and aid in CVD risk stratification in RA.
To cite this abstract in AMA style:
Federico L, Michaud K, Wipfler K, Ozen G, Baker J. Weight History and Associations with Cardiovascular Risk in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/weight-history-and-associations-with-cardiovascular-risk-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/weight-history-and-associations-with-cardiovascular-risk-in-patients-with-rheumatoid-arthritis/