Session Information
Date: Monday, November 9, 2020
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Healthcare claims databases can be used to identify patients with ankylosing spondylitis (AS) prior to diagnosis. This study explores differences in pathways to AS diagnosis between men and women by examining the coding of health events over the 2 years prior to AS diagnosis.
Methods: This retrospective cohort study collected administrative claims data from patients in the Truven Health MarketScan® Commercial and Medicare Supplemental Databases from January 2006 to April 2019. The AS population included all patients aged ≥ 18 years with ≥ 2 diagnoses of AS (ICD-9-CM/ICD-10-CM) ≥ 30 days apart who had ≥ 2 years of continuous enrollment prior to first AS diagnosis. Male patients with AS were matched 1:1 to female patients with AS by age, date of AS diagnosis, insurance type, and enrollment duration. Diagnosis codes and physician types were examined over the 2 years prior to AS diagnosis and stratified by men vs women. A set of 1906 AS-related codes in men and women was examined using univariate χ2 tests.
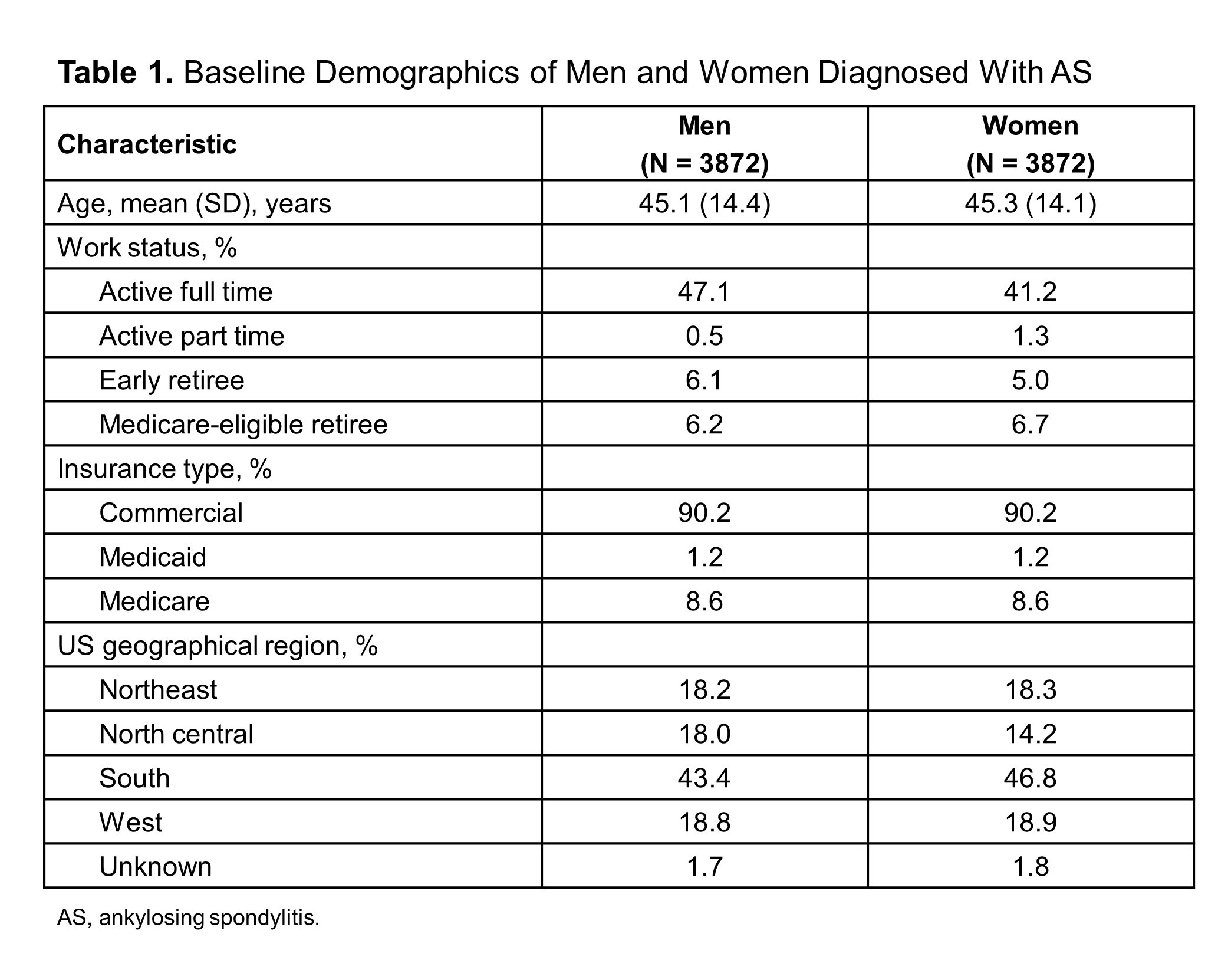
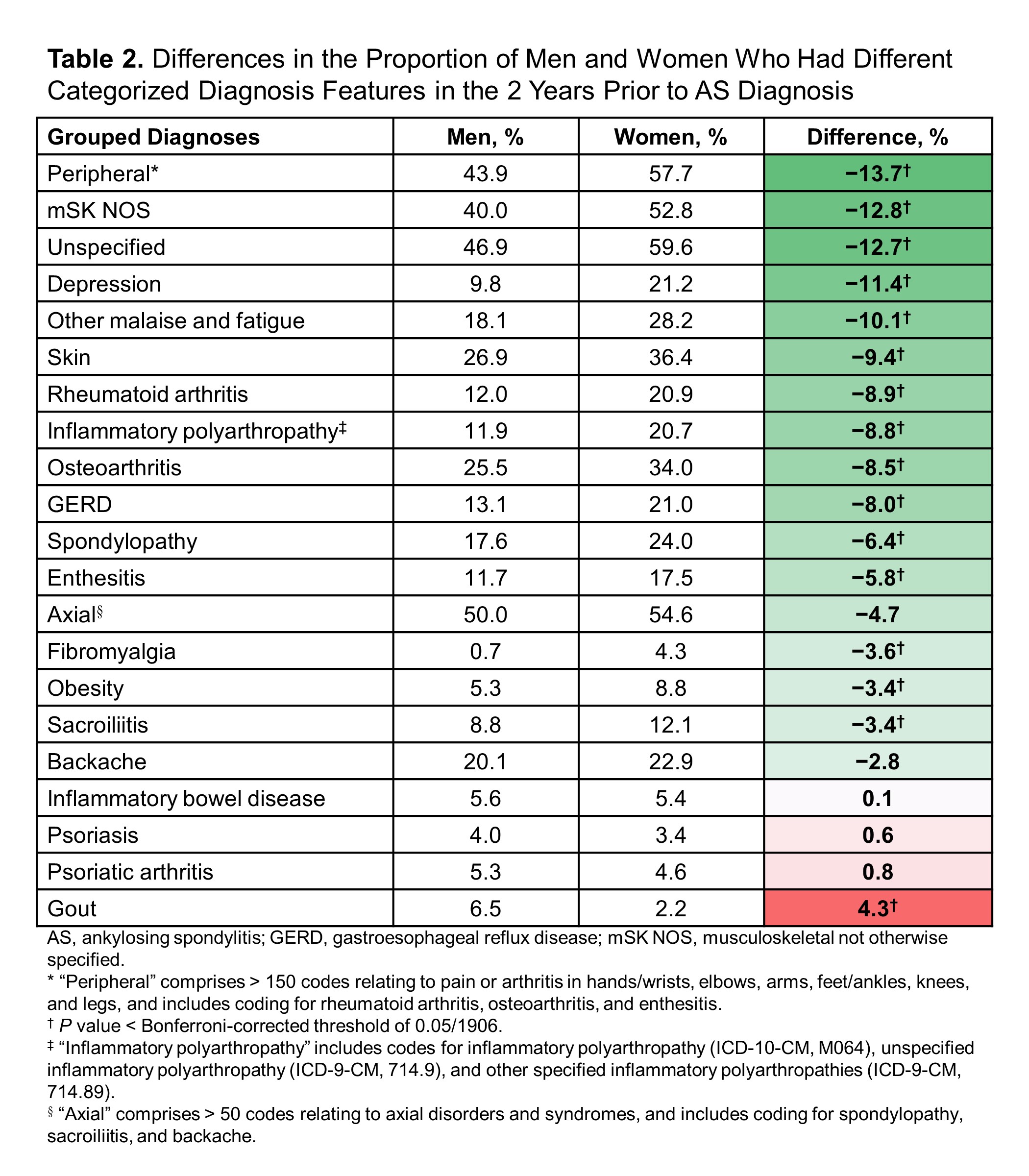
Results: A total of 7744 patients met the inclusion criteria for diagnosis of AS. The mean (SD) age for men and women, respectively, was 45.1 (14.4) and 45.3 (14.1) years; women were less likely than men to be working full time (41.2% vs 47.1%) (Table 1). Of 1906 codes examined for differences between men and women, 281 codes showed significant differences, some of which are highlighted in Tables 2 and 3. In general, women had more overall coding than men across diagnoses and providers. The greatest difference between men and women in categorized disease features was observed for peripheral symptom coding (57.7% of women vs 43.9% of men) (Table 2). Compared with men, women also showed much greater levels of other MSK coding (52.8% vs 40.0%), unspecified coding (59.6% vs 46.9%, and depression (21.2% vs 9.8%). Only gout was significantly more common in men vs women (6.5% vs 2.2%). These differences were observed throughout the 2 years prior to AS diagnosis. However, coding for backache gradually increased in men starting at 12 months before AS diagnosis, whereas axial and sacroiliitis coding increased sharply in men immediately before AS diagnosis, suggesting differences between men and women in pathways to AS or in presentation of disease. When looking at physician types visited in the 2 years prior to AS diagnosis, the greatest difference was observed for rheumatologists (64.2% of women vs 45.1% of men; difference = 19.1%) (Table 3).
Conclusion: This analysis revealed differences between men and women in the time leading up to diagnosis of AS, with the greatest variations observed for peripheral vs axial coding, unspecified coding, MSK symptoms, and depression. These findings, over a range of codes, are consistent with differences in disease phenotype between men and women that result in divergent pathways to diagnosis of AS. Women showed greater levels of coding regardless of the code being examined. A greater number of visits to community rheumatologists for women vs men support the hypothesis that there is a greater challenge in diagnosing the AS disease spectrum in women vs men by clinicians, which merits further investigation. These differences potentially contribute to a delayed, burdened journey to diagnosis of AS in women compared to men.
To cite this abstract in AMA style:
Hwang M, Rozycki M, Arndt T, Yi E, Weisman M. Differences Between Men and Women in the Patient Pathways to Diagnosis of Ankylosing Spondylitis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/differences-between-men-and-women-in-the-patient-pathways-to-diagnosis-of-ankylosing-spondylitis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-between-men-and-women-in-the-patient-pathways-to-diagnosis-of-ankylosing-spondylitis/