Session Information
Date: Monday, November 9, 2020
Title: SLE – Treatment Poster II
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
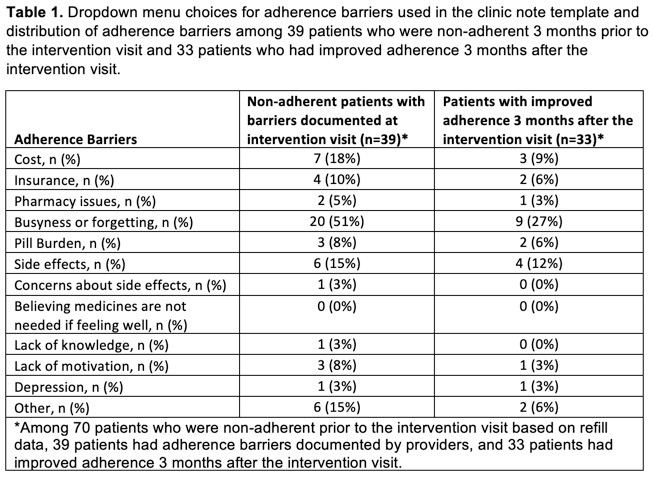
Background/Purpose: Medication non-adherence in SLE is as high as 80%, yet little is known about adherence barriers faced by patients or interventions that improve adherence in SLE. We developed an intervention based on our prior study results in collaboration with lupus clinic stakeholders and pilot-tested it in a tertiary care lupus clinic. As part of the intervention, providers shared objective pharmacy refill data with patients during the encounter to elicit adherence barriers and discussed approaches to overcoming barriers. These were then documented in the clinic note via a dropdown menu with multiple choice options (Table 1). Here we describe adherence barriers elicited and approaches suggested to overcome them as noted by lupus providers during this pilot intervention.
Methods: We conducted the pilot intervention during regular clinic visits over 12 weeks on consecutive follow-up SLE patients who were prescribed ≥1 SLE medication. Adherence was assessed by medication possession ration (MPR) based on Surescripts refill data available in the EMR supplemented by phone calls to patients’ pharmacies. Adherence was assessed for the 3-month periods before and after the intervention visit, using MPR ≥80% as a cutoff for being adherent. Approaches to overcome barriers documented by providers were collected via chart review.
Results: Among 134 SLE patients seen during the intervention period, 70 (median age 40, 96% female, 66% African-American) were inconsistent at refilling at least one SLE medication (MPR < 80%). Lupus clinic providers identified and documented adherence barriers for 39 (56%) of the 70 patients with low refills. The most common barriers were busyness or forgetting (51%), cost or insurance issues (28%), side effects (15%), pill burden (8%), and lack of motivation (8%). Three months following the intervention visit, 33 (47%) of 70 patients with low refill rates now are considered adherent. There was no significant difference in the distribution of barriers between those with and without improved adherence after the intervention visit. Approaches to overcoming barriers documented by providers included: strategies to help with remembering, for example, using a reminder, app, or pill box, moving pills to a more visible area, or involving a family member to remind the patient (n=10); modifying the medication schedule or prescription (n=7); eliciting help from the pharmacist and/or social worker for cost and insurance issues (n=5); providing education or clearer instructions (n=5); treating side effects (n=2); and addressing depression (n=1).
Conclusion: We found that the most frequent medication adherence barriers faced by SLE patients related to the logistics of taking medications, financial burden, and side effects. The most common approach to address barriers suggested by providers were strategies to help with logistics of taking medications. The similar distribution of adherence barriers between those who did and did not have improved adherence after the intervention visit suggests that most of the barriers are modifiable.
To cite this abstract in AMA style:
Eder L, Clowse M, Eudy A, Rogers J, Sadun R, Criscione-Schreiber L, Doss J, Maheswaranathan M, Corneli A, Bosworth H, Sun K. Medication Adherence Barriers and Opportunities to Overcome Them Among Patients with SLE [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/medication-adherence-barriers-and-opportunities-to-overcome-them-among-patients-with-sle/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/medication-adherence-barriers-and-opportunities-to-overcome-them-among-patients-with-sle/