Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: We have noticed an increasing number of serum IgG4 levels ordered over the last several years at our institution. This study was performed to better understand the clinical indications for IgG4 testing among inpatient general medicine providers and how those trends have changed from 2015 to 2019. We also sought to determine if there was any comparative change in rheumatology providers’ behavior regarding IgG4 testing.
Methods: We used SlicerDicer, an analytic tool in our EHR, to identify patients with IgG subclasses ordered by inpatient general medicine or rheumatology providers in 2015 and 2019. Charts were manually reviewed to determine clinical indications for IgG subclass testing as determined by provider documentation at the time of ordering. Using a pre-specified adjudication algorithm, patients were excluded if IgG subsets were sent for an indication other than IgG4-Related Disease (IgG-RD) or if they already had a known diagnosis of IgG4-RD. For included patients, we also evaluated IgG4 levels, imaging, biopsies, and final diagnoses. Fisher’s exact test (Social Science Statistics open software) was used to compare 2015 and 2019 data. Other data were analyzed using descriptive statistics.
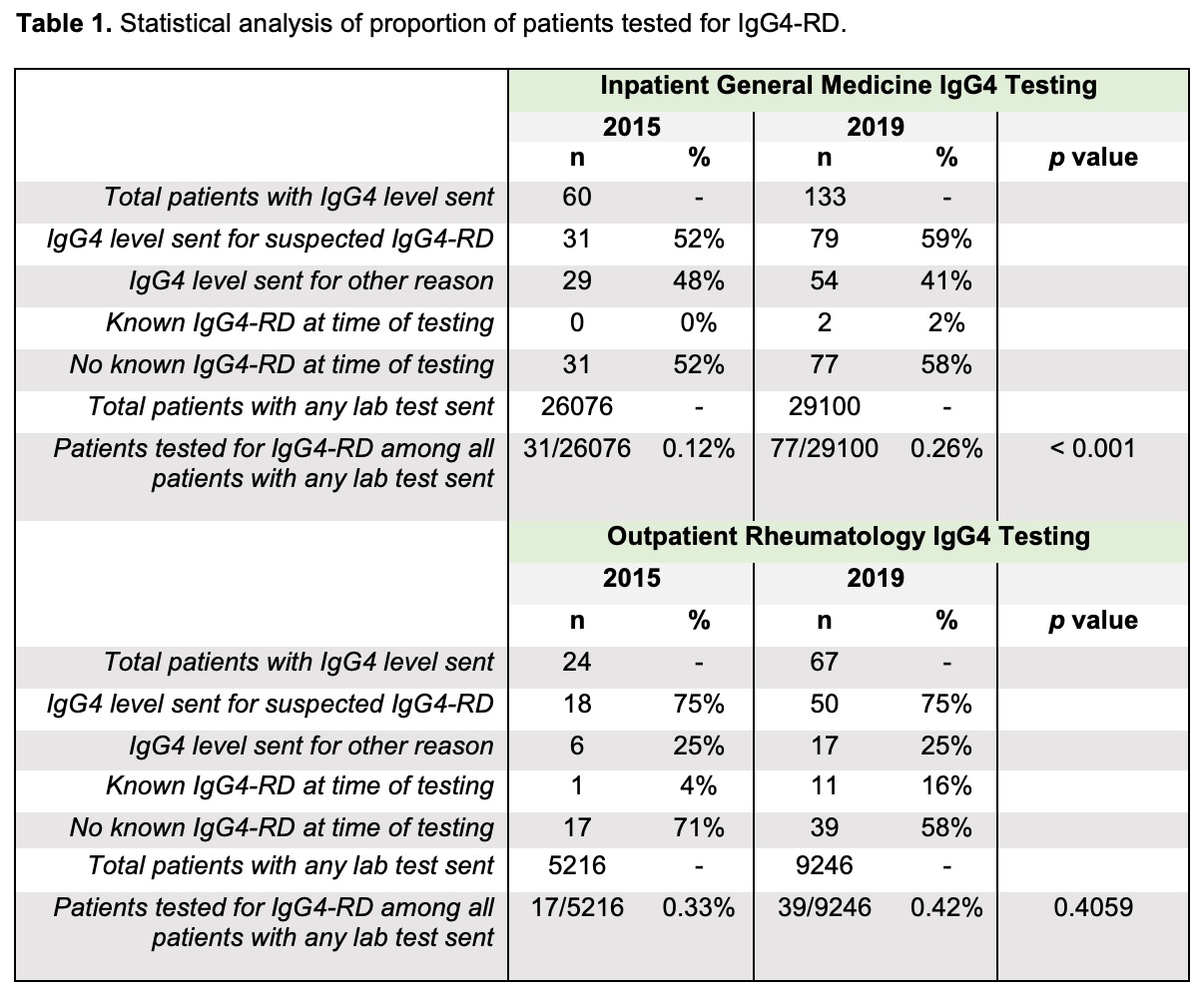
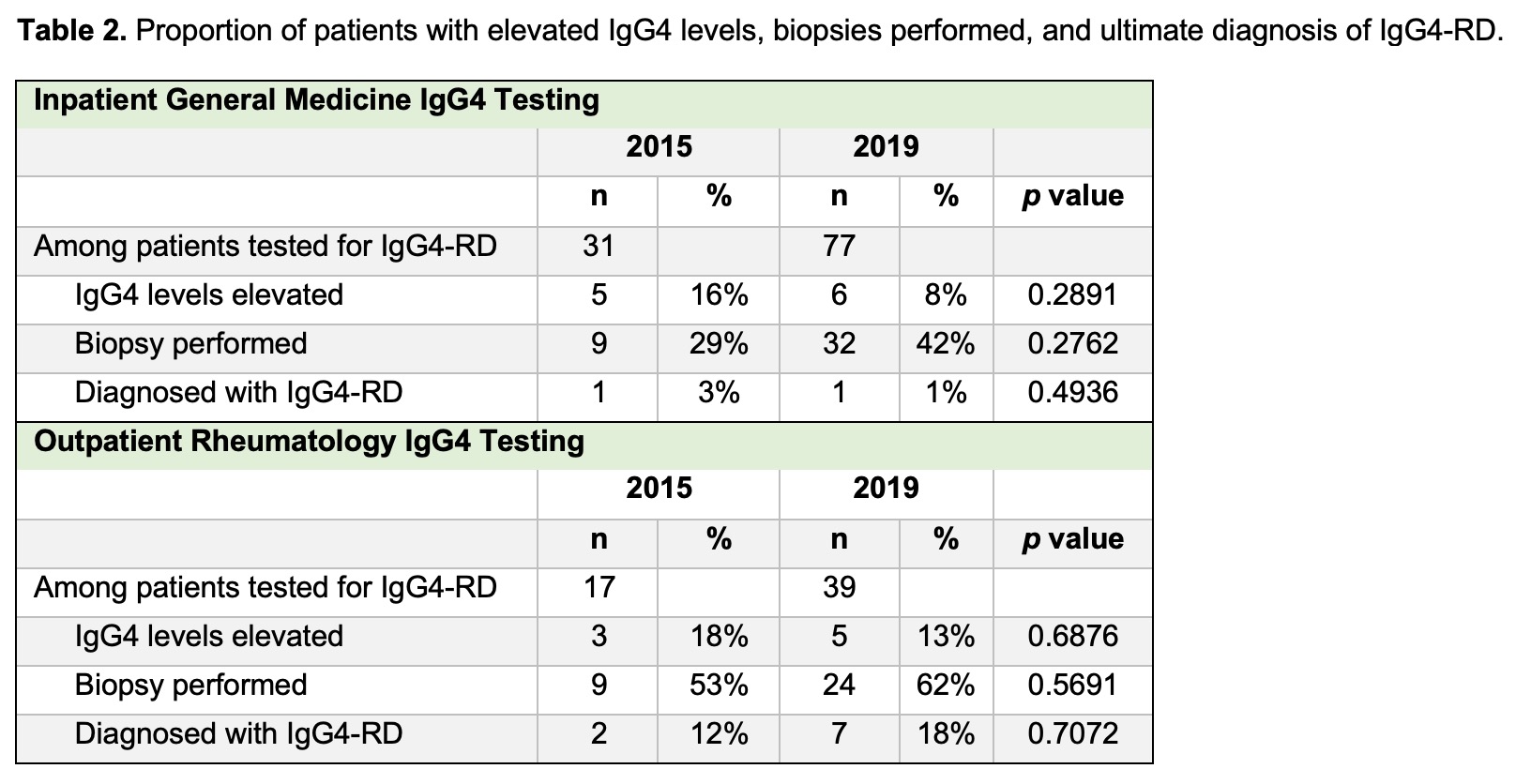
Results: Among general medicine providers, there was a significant increase in patients tested for suspected IgG4-RD with serum IgG subclasses from 2015 (n = 31, 0.12% of all patients with any lab order) to 2019 (n = 77, 0.26%), p< 0.001 (table 1). There were no changes in the proportion of patients with elevated IgG4 levels, biopsies obtained, or a diagnosis of IgG4-RD from 2015 to 2019 (table 2). Notably, only 1 general medicine patient was diagnosed with IgG4-RD in 2015 and 1 in 2019. There was a significant decrease in the proportion of general medicine patients tested with IgG subclasses for IgG4-RD due to retroperitoneal fibrosis (10% in 2015 vs 0% in 2019, p=0.022) and a trend towards more patients tested due to hepatobiliary disease (13% vs 30%, p=0.0861) and orbital inflammatory disease (0% vs 9%, p=0.0571), table 3. There were no significant changes in IgG subclass testing patterns by rheumatology providersfrom 2015 to 2019.
Conclusion: Despite a more than two-fold increase in IgG subclass testing for IgG4-RD by inpatient general medicine providers from 2015 to 2019, the number of patients ultimately diagnosed with IgG4-RD did not change. The trend towards increased IgG subclass testing for hepatobiliary disease and orbital inflammatory disease suggests increased provider awareness of some of this condition’s protean manifestations beyond the pancreas; however, the decrease in IgG subclass testing for retroperitoneal fibrosis and the minimal testing for other major clinical manifestations of IgG4-RD in either 2015 or 2019 suggests that this condition remains under-recognized. In contrast, there were no major changes in IgG subclass testing by rheumatologists from 2015 to 2019. Overall, this study reveals potential knowledge gaps regarding the workup of IgG4-RD among inpatient internal medicine providers and highlights the need for an educational intervention to address appropriate indications for IgG subclass testing in different clinical scenarios.
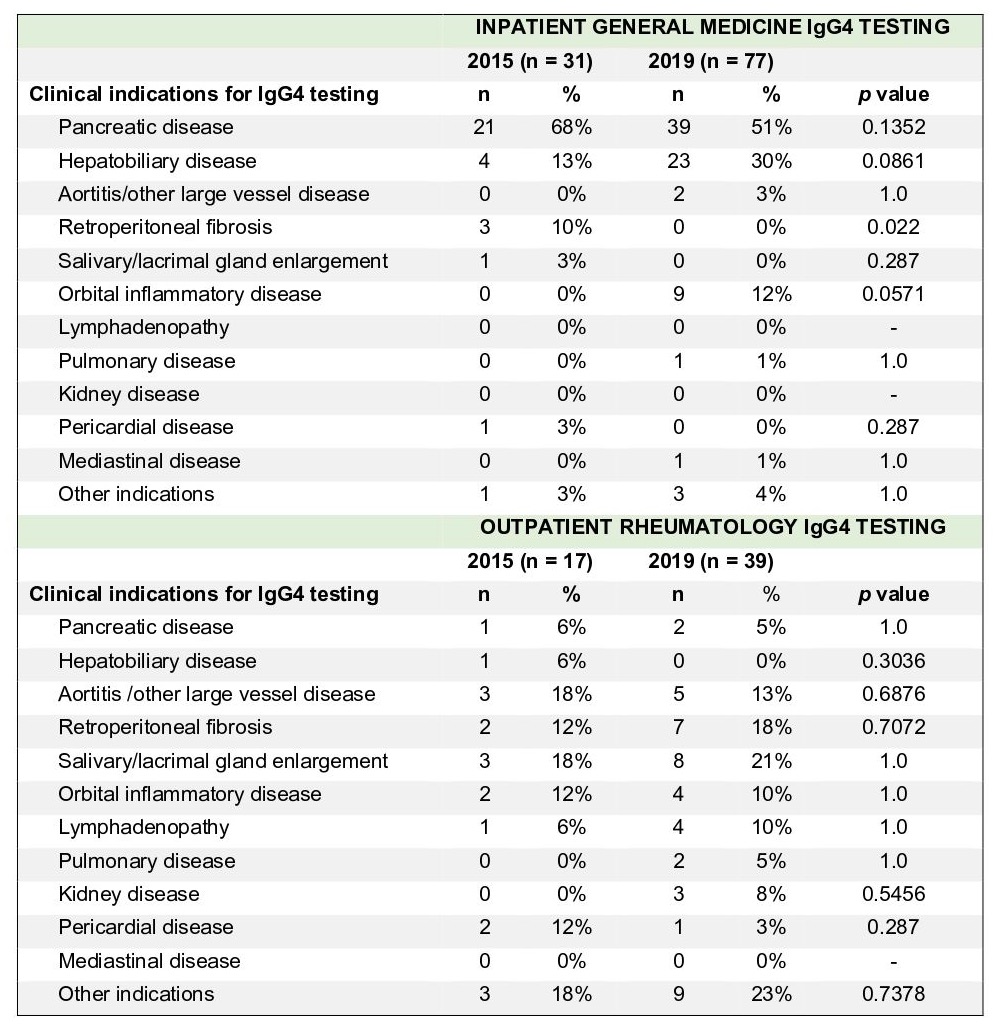 Table 3. A review of clinical characteristics and indications of patients tested for IgG4-RD.
Table 3. A review of clinical characteristics and indications of patients tested for IgG4-RD.
To cite this abstract in AMA style:
Eder L, Leverenz D. Immunoglobulin G Subclass Ordering Patterns for IgG4-Related Disease at an Academic Medical Center [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/immunoglobulin-g-subclass-ordering-patterns-for-igg4-related-disease-at-an-academic-medical-center/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/immunoglobulin-g-subclass-ordering-patterns-for-igg4-related-disease-at-an-academic-medical-center/