Session Information
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: Rheumatic and musculoskeletal diseases (RMDs) often predispose the development of other chronic conditions, resulting in multimorbidity. While multimorbidity is increasingly being recognized and examined within individual RMDs, few studies have directly compared the burden and pattern of multimorbidity across RMDs. Therefore, we aimed to compare multimorbidity between rheumatoid arthritis (RA), psoriatic arthritis (PsA), gout, and osteoarthritis (OA) within the Rheumatology Informatics System for Effectiveness (RISE) registry.
Methods: We conducted a cross-sectional study within the RISE registry, the largest EHR-enabled rheumatology registry in the U.S. We selected patients >18 years of age, with ≥2 RISE encounters over ≥30 days, and who fulfilled algorithms for RA, PsA, gout, or OA (≥2 consecutive visits with corresponding ICD-10 codes) in a hierarchical fashion to avoid patients contributing to multiple disease groups. Multimorbidity was assessed using the RxRisk, a medication-based index of chronic conditions, assessed using all available preceding data before the 2nd visit. We compared the frequency of multimorbidity (defined as receiving medications from ≥5 different RxRisk categories; Wallace E. et al. BMJ Open, 2016) across disease groups using multivariable logistic regression and the burden of multimorbidity (defined as the number of RxRisk categories) using multivariable negative binomial regression.
Results: We included 356,820 patients from the RISE registry (n=152,214 RA, n=33,156 PsA, n=19,781 gout, n=151,669 OA) with characteristics shown in Table 1. Patients with PsA were younger and more frequently Caucasian while male sex was more frequent in patients with gout or PsA. The odds of multimorbidity (³5 RxRisk categories) were 1.29-fold higher in gout than RA (95% CI 1.23-1.34; Table 2). Compared to patients with RA, the prevalence of multimorbidity was similar in PsA (p=0.15) but less frequent in OA (OR 0.78, 95% CI 0.76-0.79). Similarly, a higher burden of multimorbidity (# of RxRisk categories) was observed in gout compared to RA (B=0.054, P< 0.001; Table 2). Both PsA (B=-0.008, P=0.02) and OA were associated with a lower burden of multimorbidity than RA (B=-0.086, P< 0.001). Distinct patterns of multimorbidity were noted across disease groups. Specifically, metabolic and cardiac RxRisk categories were most closely associated with gout, while thyroid and osteoporosis categories were most closely associated with RA and OA.
Conclusion: In this large, national, U.S. rheumatology EHR-based registry, multimorbidity was highly prevalent in RA, PsA, gout, and OA. Recognizing the tremendous burden and unique patterns of multimorbidity accompanying these conditions is an essential step for optimizing the management of RMDs in real-world populations.
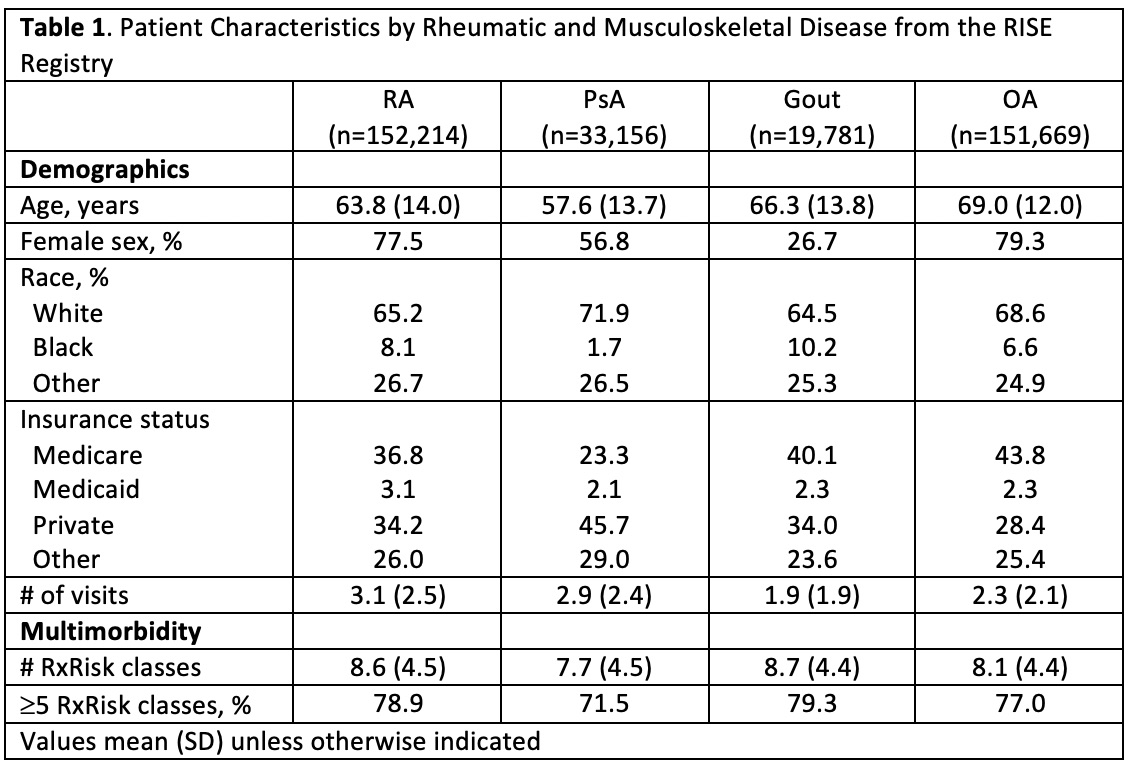 Table 1. Patient Characteristics by Rheumatic and Musculoskeletal Disease from the RISE Registry
Table 1. Patient Characteristics by Rheumatic and Musculoskeletal Disease from the RISE Registry
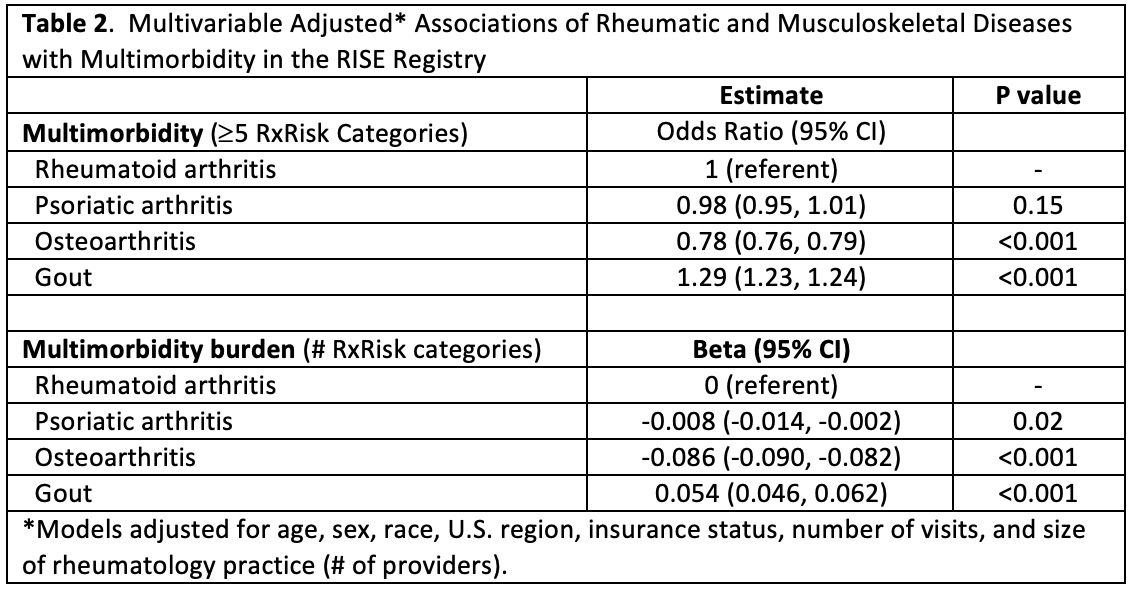 Table 2. Multivariable Adjusted Associations of Rheumatic and Musculoskeletal Diseases with Multimorbidity in the RISE Registry
Table 2. Multivariable Adjusted Associations of Rheumatic and Musculoskeletal Diseases with Multimorbidity in the RISE Registry
To cite this abstract in AMA style:
England B, Yun H, Chen L, Michaud K, Mikuls T, Curtis J. Multimorbidity in Rheumatoid Arthritis, Psoriatic Arthritis, Gout, and Osteoarthritis Within the Rheumatology Informatics System for Effectiveness (RISE) Registry [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/multimorbidity-in-rheumatoid-arthritis-psoriatic-arthritis-gout-and-osteoarthritis-within-the-rheumatology-informatics-system-for-effectiveness-rise-registry/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multimorbidity-in-rheumatoid-arthritis-psoriatic-arthritis-gout-and-osteoarthritis-within-the-rheumatology-informatics-system-for-effectiveness-rise-registry/
