Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) patients have a prominent neutrophil gene expression signature. However, investigations into the pathophysiologic role of neutrophils in SSc are lacking. This is predominantly due to their limited survivability in vitro and the significantly lower proportion of neutrophils in rodent serum compared to humans. These limitations highlight the need to directly study the role of neutrophils in SSc using human specimens. In this study, we examined the prognostic significance of neutrophil count in the Scleroderma Lung Study (SLS) II.
Methods: Neutrophil counts were prospectively obtained at the baseline visit of SLS II. All subjects had clinically significant SSc related interstitial lung disease (ILD) and had a disease duration less than 7 years. Baseline neutrophil count was log-transformed with a base of 2 in all analyses. A joint model combining mixed effects and survival models was used to examine the relationship between baseline blood neutrophil count and serially obtained % predicted forced vital capacity (FVC%) as well as modified Rodnan skin scores (mRSS) from 3-12 month visits after adjustment for baseline disease severity and treatment arm. Cox proportional hazards models were created to evaluate the association between neutrophil count and long-term mortality.
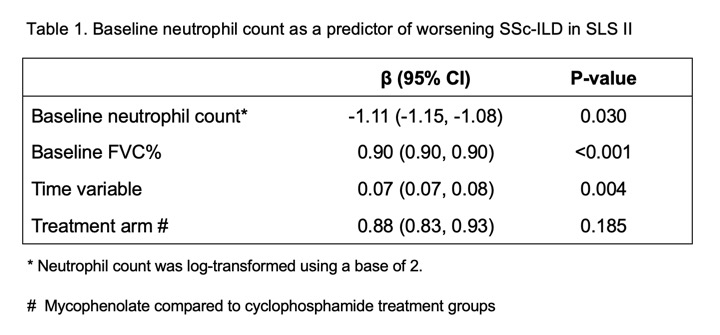
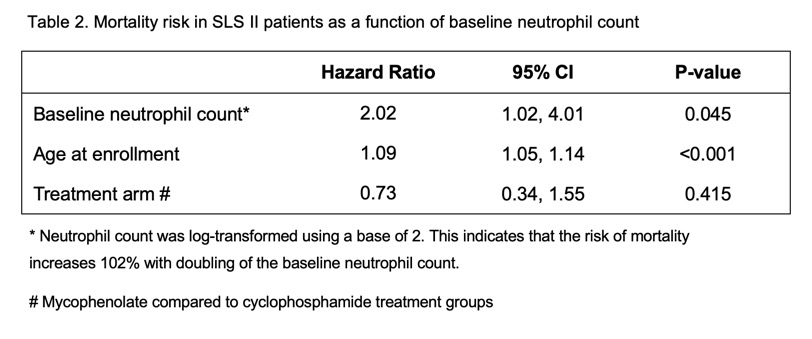
Results: Of the 142 patients enrolled in SLS II, 134 (94.3%) had an available baseline neutrophil count. The majority of patients had diffuse cutaneous disease (59%) and mean disease duration was 2.6 years (±1.7). Higher neutrophil count predicted worsening of SSc-ILD based on the course of the FVC% from 3-12 months (p=0.030 – Table 1). Neutrophil count did not predict changes in mRSS. Baseline neutrophil count predicted an increased risk of mortality after adjustment for age (HR=2.02, 95% CI [1.02, 4.01], p=0.045-Table 2). The median follow-up time was 3.4 years with IQR (2.9, 4.6) for the mortality analysis. Both findings were independent of treatment arm.
Conclusion: Higher neutrophil count predicted worse ILD course and higher long-term mortality in patients with SSc-ILD. Our findings were independent of treatment with cyclophosphamide or mycophenolate. Neutrophils, largely under-investigated in SSc, might play a role in pathogenesis of SSc and warrant further mechanistic studies. Furthermore, baseline neutrophil counts may serve as a useful prognostic marker of disease progression.
To cite this abstract in AMA style:
Wareing N, Li N, Volkmann E, Lyons M, Roth M, Tashkin D, Assassi S. Serum Neutrophil Count Predicts Progression of Interstitial Lung Disease and Mortality in Patients with Systemic Sclerosis Related Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/serum-neutrophil-count-predicts-progression-of-interstitial-lung-disease-and-mortality-in-patients-with-systemic-sclerosis-related-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-neutrophil-count-predicts-progression-of-interstitial-lung-disease-and-mortality-in-patients-with-systemic-sclerosis-related-interstitial-lung-disease/