Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Bone Replaces Cartilage In Non-Weight Bearing Regions Of Immobilized Knees
Background/Purpose:
Osteoarthritis causes pain, restricts joint range of motion, reduces function, is highly prevalent worldwide and contributes to an ever-increasing burden on global health care costs1. Joint immobility damages articular tissues including cartilage, and has been used as an experimental model for OA2, 3. Various immobilization models in animals have been used including use of straps/slings, splints/casts, or rigid external fixation with or without weight-bearing on the immobilized joint, a crucial factor in articular homeostasis4. Therefore, the pathophysiology of immobility-related cartilage alterations and hence directions for treatment would still benefit from new data. This study examined the effect of knee joint immobilization in flexion on tibial epiphysis articular cartilage, comparing weight-bearing and non-weight-bearing regions.
Methods:
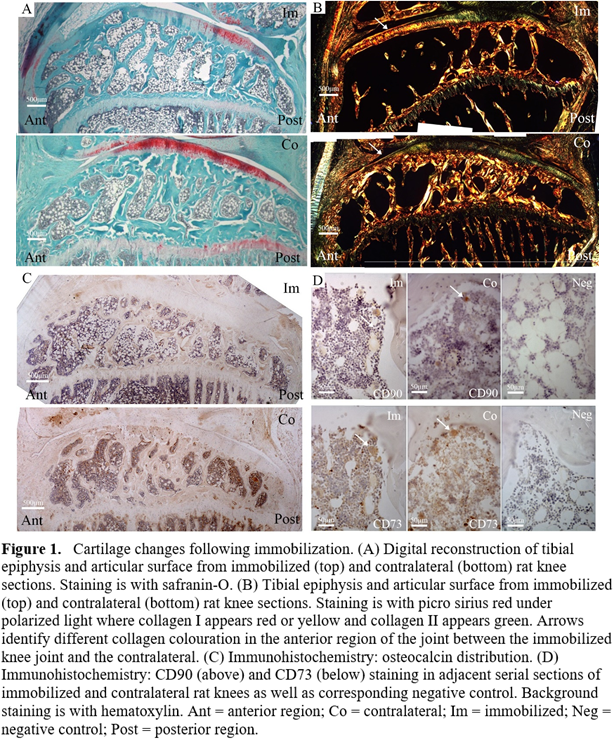
Eleven rat knees were rigidly immobilized for 32 weeks at 135° of flexion. Contralateral limbs served as controls. The medial tibial epiphysis on histological sagittal sections was divided into non-weight-bearing (anterior) and weight-bearing (middle, posterior) regions on digital images. We quantified cartilage thickness and glycosaminoglycan (GAG) staining intensity using safranin O, as well as the distribution of collagen I and II using picrosirius red under polarized light. We evaluated osteoblast activity and the presence of mesenchymal stem cells (MSCs) using immunohistochemistry to osteocalcin and overlapping CD90 and CD73 staining on serial sections, respectively.
Results:
Immobilized mean cartilage thickness was reduced in the anterior region but increased in the posterior region (92±68μm, 235±56μm respectively, Figure 1A top) compared to contralateral (154±49µm, p=0.022; 186±48µm, p<0.001, respectively, Figure 1A bottom). GAG cartilage staining area was 2±4% in the anterior region of immobilized knees compared to 28±12% contralaterally (p=0.003). Immobilized knees had decreased collagen II staining area (11±9% vs 36±12%, p=0.006) and increased collagen I staining area (61±20% vs 43±12%, p=0.033) in the anterior cartilage region (Figure 1B top). Osteocalcin (Figure 1C) and MSC staining (Figure 1D) were decreased in immobilized knees (p=0.003 and p=0.036 for CD90 only, respectively) with no significant inter-regional differences.
Conclusion:
After 32 weeks of knee immobilization, the non-weight-bearing region of the tibia articular cartilage was thinner, lost GAG, and was replaced by bone. Long-duration immobility may share pathophysiologic features with OA and should be intervened upon in earlier stages.
References :
S. J. Nho, S. M. Kymes, et al., 2013.
T. Videman, J. E. Michelsson, et al., 1976.
H. I. Michelsson JE, 1984.
A. J. Teichtahl, A. E. Wluka, et al., 2015.
To cite this abstract in AMA style:
Campbell TM, Reilly K, Laneuville O, Uhthoff H, Trudel G. Bone Replaces Cartilage in Non-Weight Bearing Regions of Immobilized Knees [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/bone-replaces-cartilage-in-non-weight-bearing-regions-of-immobilized-knees/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-replaces-cartilage-in-non-weight-bearing-regions-of-immobilized-knees/