Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Burnout, a syndrome of emotional exhaustion, has adversely impacted the delivery of high-quality, compassionate care across healthcare settings for years. While physicians have higher resilience compared to the general population and higher resilience scores have been associated with lower burnout rates, even the most resilient physicians have been found to have substantial burnout rates. In response to a paucity of existing data, we aimed to measure baseline levels of wellness, resilience, and burnout among pediatric rheumatology fellows prior to participation in a narrative medicine intervention for future study.
Methods: This study involved a cross-sectional survey of pediatric rheumatology fellows in the US and Canada who consented to participate in a narrative medicine intervention. Survey components included the Mini Z Burnout Survey, Mayo Well-being Index and Connor-Davidson Resilience Scale (CD-RISC), as well as baseline demographics and self-reported burnout-related factors. Measured burnout-related factors included time on call, outpatient clinic, joint injections, workplace culture and environment, colleagues and supervisors, salary, career growth, development and research, commuting and sleep.
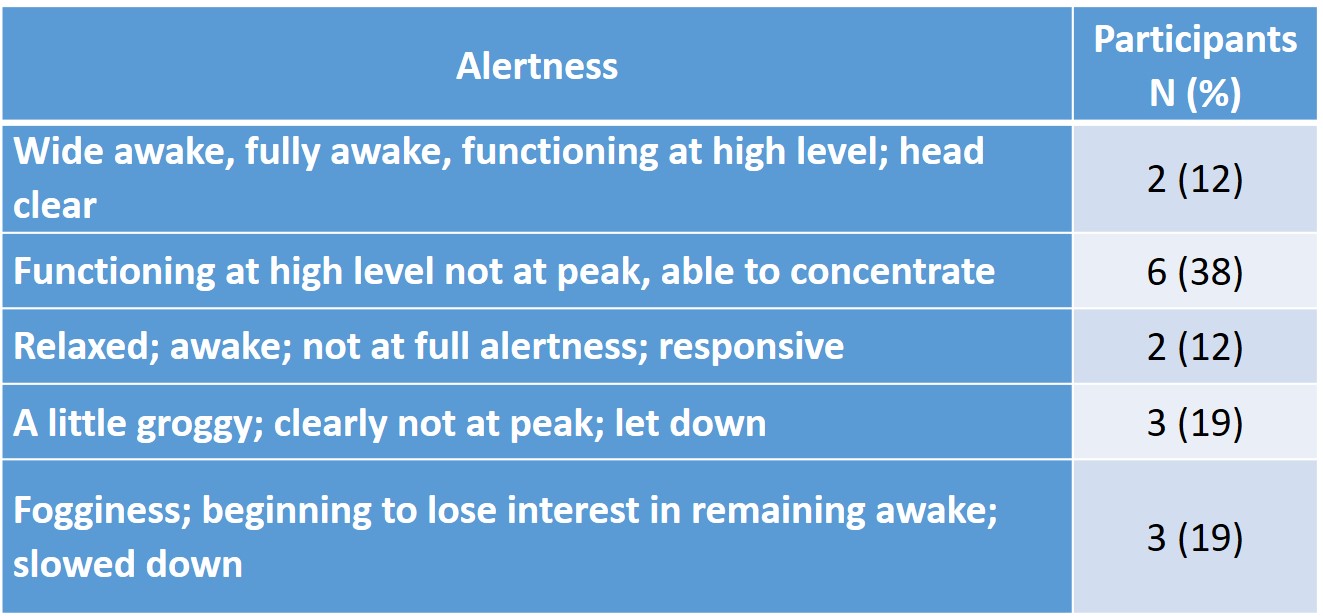
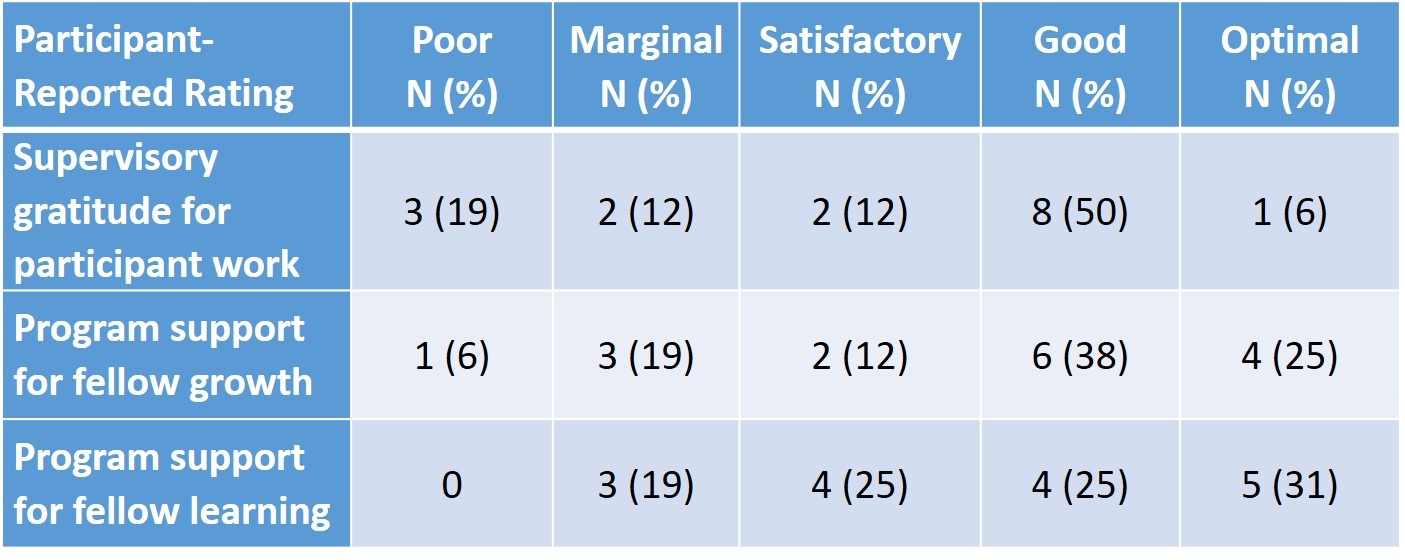
Results: All invited sixteen fellows completed the survey, including one fourth year fellow, four third year fellows, four second year fellows and seven first year fellows. The median (range) CD-RISC resilience score was 73.5 (44-88), with high resilience considered to be scores over 25.5. The Mini-Z Burnout showed high levels of burnout with a median (range) of 34 (17-44). A statistically significant Spearman’s correlation was observed between resilience and burnout, where higher resilience correlated with lower burnout (r=0.5, p= 0.03). Spearman’s correlation also showed that worse wellness scores correlated with worse burnout scores (r=-0.8 p=0.006), and better wellness scores correlated with higher rates of resilience (r=-0.6, p=0.02). The median (range) score of the Mayo Wellbeing Index was 3 (0-7), with scores of ≥ 4 associated with physicians at risk of adverse consequences such as suicidal ideation and/or serious thoughts of leaving medicine. Participants reported a median (range) of 7 (5.5-7) hours of sleep per night, and only 12% reported feeling wide awake with a clear head (Table 1). Sixty-nine percent reported feeling no control over clinic schedules. Two thirds felt their workplace had a good culture. Three quarters felt leadership communicated effectively, and 63% felt they were able to express concerns and frustrations to leadership. Eighty one percent felt supported by colleagues and supervisors, and 88% liked their colleagues and supervisors. Table 2 shows participant-reported ratings of both supervisory gratitude for participant work and program support for career growth and learning.
Conclusion: This study demonstrates baseline levels of wellness, resilience and burnout among pediatric rheumatology fellows. This data offers new insight into the rising pediatric rheumatology workforce and may offer areas to target for future interventions that can mitigate burnout and maximize resilience among fellows.
To cite this abstract in AMA style:
Lanis A, Spitznagle J, Cook K, Vora S, Hays K, Murphy Schmidt K, Bartley A, Moorthy L, Wells C. Wellness, Resilience and Burnout Among Pediatric Rheumatology Fellows [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/wellness-resilience-and-burnout-among-pediatric-rheumatology-fellows/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/wellness-resilience-and-burnout-among-pediatric-rheumatology-fellows/