Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Intra-articular injections (IAI) are commonly used to relieve pain and delay total knee replacement (TKR) in persons with knee OA. Despite higher costs and conflicting evidence of efficacy, utilization of hyaluronic acid (HA) and platelet rich plasma (PRP) IAIs have increased dramatically over the last decade.
Methods: We used the Osteoarthritis Policy (OAPol) Model, a widely published and validated microsimulation of knee OA, to assess the value of alternative IAIs. We considered 5 strategies: 1) no IAI, 2) saline (placebo), 3) corticosteroid (CS), 4) HA, and 5) PRP. We assumed that IAIs are offered to patients with inadequate pain control from NSAIDs. In the model, if and when IAIs do not provide adequate pain relief, OA care progresses to opioids and/or TKR. We used a random-effects meta-analysis to estimate IAI-specific pain reduction from high-quality (Jadad score 4+) RCTs. We analyzed data from 11 RCTs for saline, 12 for CS, 24 for HA, and 8 for PRP. We estimated pain reductions for one IAI series of -14 points for saline at 3 months, -22 for CS at 3 months, -22 for HA at 6 months, and -17 for PRP at 12 months. The cost of IAIs included the visit, IAI administration and medication costs. We derived the cost of CS ($315), HA ($795), and saline ($309) IAI from the Medicare Drug Fee Schedule and estimated the cost of PRP ($2586) from literature. In the base case analysis, based on the literature, we assumed that repeat CS injections increase the risk of OA progression (HR=3.02). We ran the model over the remaining lifetime of a cohort with average age 50 years at the start of simulation, pain 51 (WOMAC, 0-100, 100 worst), 50% KL3/50% KL2. We determined the value of specific IAIs using incremental cost-effectiveness ratios (ICERs), evaluated from the health care perspective and calculated as the ratio of the difference in lifetime costs to the difference in quality adjusted life years (QALYs) between two strategies. The IAI that maximizes QALYs with ICER< willingness to pay (WTP) threshold is considered the most cost-effective strategy.
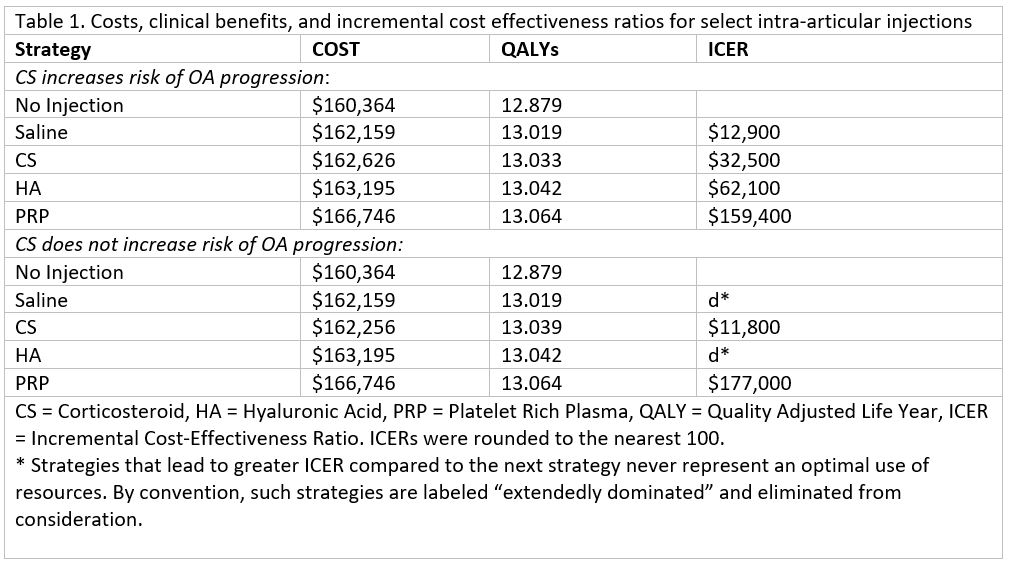
Results: QALYs and costs for each strategy are presented in Table 1. Assuming CS does not increase the risk of OA progression, CS results in an ICER of $11,800/QALY compared to no injection, and PRP results in an ICER of $177,000/QALY compared to CS. Assuming CS does increase the risk of OA progression, the resultant ICERS are $12,900/QALY for saline compared to no injection, $32,500/QALY for CS compared to saline, $62,100/QALY for HA compared to CS, and $159,400/QALY for PRP compared to HA. If CS increased the risk of OA progression, PRP would achieve ICERs of $100K/QALY ($50K/QALY) at a price of $1,965 ($1,448). If CS did not increase risk of OA progression, even lower PRP prices ($1,655 and $1,086) would be required to attain these ICER thresholds.
Conclusion: For WTP thresholds between $11,800 and $62,100/QALY, CS is the preferred strategy, regardless of what we assume about their impact on OA progression. If CS has no impact on risk of OA progression, it remains the preferred strategy until WTP exceeds $177,000/QALY. If CS increases risk of OA progression, HA becomes preferred for WTP > $62,000.
To cite this abstract in AMA style:
Mass H, Collins J, Hunter d, Yang C, Jones M, Messier S, Neogi T, Paltiel A, Katz J, Losina E. Value of Various Intra-Articular Injections for Knee Osteoarthritis Management [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/value-of-various-intra-articular-injections-for-knee-osteoarthritis-management/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/value-of-various-intra-articular-injections-for-knee-osteoarthritis-management/