Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: The incidence of lung disease within the rheumatoid arthritis is well described and likely underestimated. Additionally, RA patients are at higher risk for developing significant infections (SI).
In our own cohort the most common infections recorded were respiratory tract infections (RTI) and this was most likely to lead to increased mortality. This accords with studies showing that hospitalisations from pneumonia are higher in RA cohort compared to matched cohorts.
To determine if pre-existing subclinical functional or structural lung disease had an association with an increased risk of respiratory tract infections, including viral pneumonias, as opposed to other infections.
Methods: All patients in our tertiary hospital RA cohort, in the last 3 years, who had any SI were included. The patient’s medical history was examined to determine if they had evidence of functional or structural lung damage prior to the infection using imaging records and previous pulmonary function tests. Patients presenting to hospital, or their general practitioner, and their diagnosis on discharge was either community acquired pneumonia, viral respiratory tract infection or other lower respiratory tract infection were included. Patients with RTI were compared to a sample of patients with RA and any non-respiratory SI (Table 1).
A Chi-Square analysis was used to compare the groups. The two groups were matched for daily steroid use, smoking history and vaccination status, there was no statistical difference between these two groups.
Results: 142 patients were identified as having an SI in the past 3 years in our cohort. 48 patients developed RTI and 94 patients who developed other infections including Urinary traction infections, skin and soft tissue infections. Of the 48 who developed RTI, 32 had evidence of subclinical lung disease compared to 16 with no evidence of lung disease. Of the 94 who developed other SI, only 21 had evidence of subclinical lung disease compared to 73 with no evidence of subclinical lung disease (Table 2).
A Chi-Square analysis of the data was performed
X2 = (1, N = 142) = 23.84, p < 0.001
allowing us to consider that pre-existing lung disease may be involved in this subset of RA patients being more susceptible to LRTIs. Patients with known pre-existing lung disease where excluded from this analysis.
Conclusion: A greater number of patients within the RTI group had previous lung abnormality compared to patients in the non-pulmonary infection group. This supports evolving literature that even subclinical lung abnormality should be considered within the suite of risk factors for RTI risk in RA.
Given the current climate and fear surround viral pneumonias, screening this cohort will allow for better risk stratification and management of these patients. This may include early admission and intervention or, in the outpatient setting, highlight the need for discussion around vaccinations to reduce this risk.
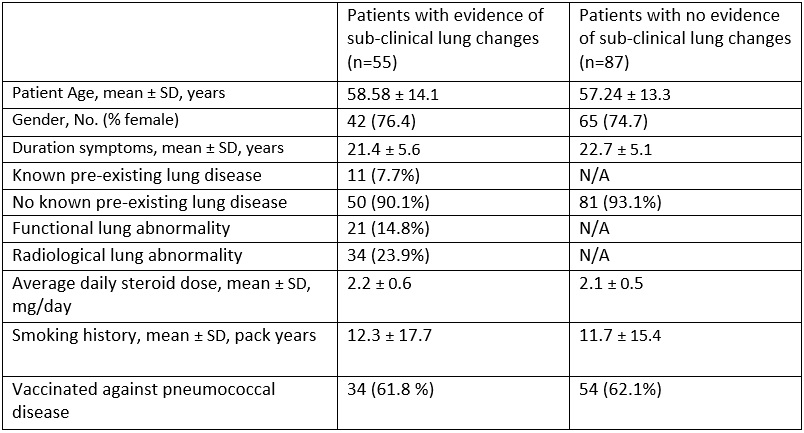 Table 1: Patient demographics and selected investigations (n =142)
Table 1: Patient demographics and selected investigations (n =142)
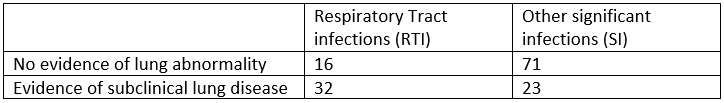 Table 2: Type of infections suffered and evidence of subclinical lung disease (n = 142)
Table 2: Type of infections suffered and evidence of subclinical lung disease (n = 142)
To cite this abstract in AMA style:
Worcester B, Wang D, Morton S, Leech M. Unrecognised, Subclinical, Structural or Functional Lung Changes in Rheumatoid Arthritis Is Associated with a Higher Risk of Developing Serious Respiratory Tract Infection [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/unrecognised-subclinical-structural-or-functional-lung-changes-in-rheumatoid-arthritis-is-associated-with-a-higher-risk-of-developing-serious-respiratory-tract-infection/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/unrecognised-subclinical-structural-or-functional-lung-changes-in-rheumatoid-arthritis-is-associated-with-a-higher-risk-of-developing-serious-respiratory-tract-infection/
