Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Understanding glucocorticoid (GC) exposure is critical for observational analyses in rheumatology. However, obtaining an accurate measure of GC exposure, including dosage and duration, has been challenging, particularly using electronic health record (EHR) data. In this study, we compared GC medication data derived from the EHRs of 234 rheumatology practices to corresponding Medicare claims for patients with rheumatoid arthritis (RA).
Methods: Data derived from RISE, a national, EHR-enabled registry that passively collects data on all patients seen by participating rheumatology practices, and linked Medicare Part D claims. We included patients ≥ 18 years with RA (≥ 2 visits with RA codes ≥ 30 days apart) with oral GCs documented in both the EHR and Medicare during 2018. We extracted GC records from 3 sources: EHR e-prescriptions (orders), EHR medication lists (“med list”), and Medicare claims. GCs were identified using NDC codes and brand and generic names; all doses were converted to prednisone equivalents. EHR records with missing stop dates (37% of e-prescription records and 86% of med list records) were assumed to last 90 days. GC records from each data source were aggregated to the patient level and daily dose was calculated as the sum of all GC records active on a given day. Daily doses were averaged over 365 days to calculate an average daily dose during 2018.
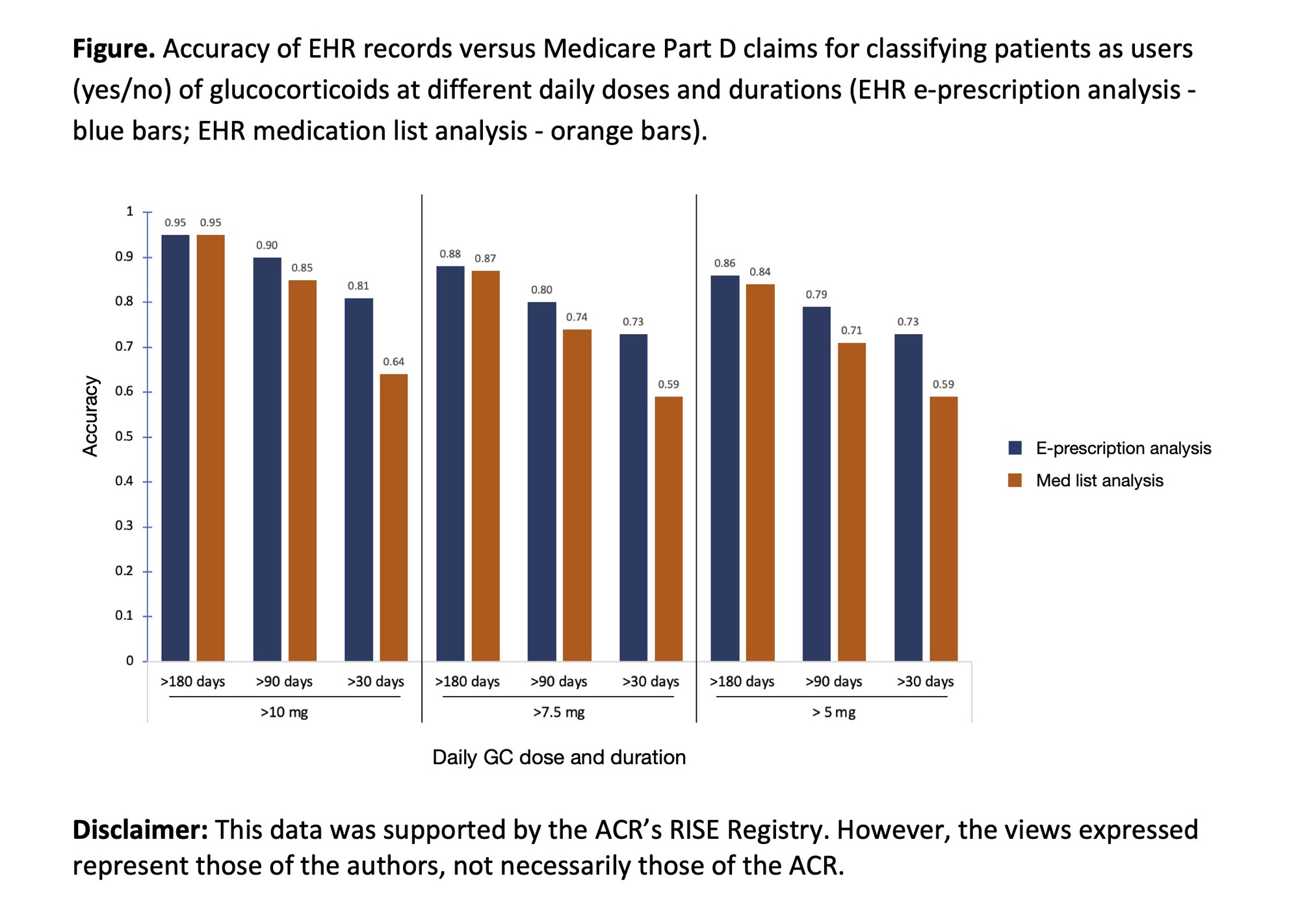
We compared GC exposure calculated from 1. EHR e-prescriptions with Medicare claims (from RISE prescribers only); and among those patients for whom e-prescription data was not available, 2. EHR med lists with Medicare claims (from any prescriber). We calculated the accuracy of EHR records vs. Medicare claims for classifying patients as users (yes/no) of GC at different daily doses and durations.
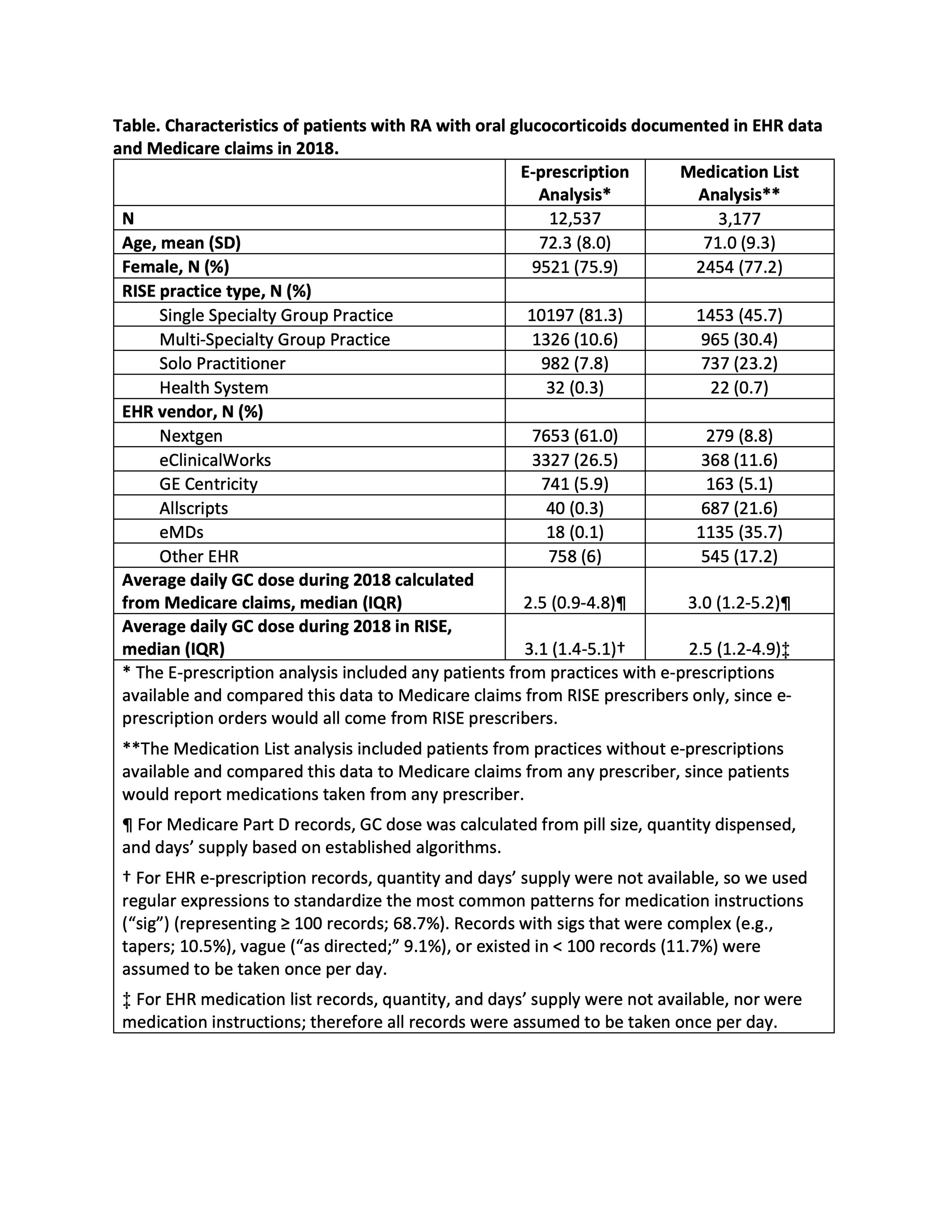
Results: We included 12,537 patients with RA in the e-prescription analysis and 3,177 in the med list analysis (Table). Both groups had similar demographics ( >75% female, mean (SD) age 72.3 (8.0) years) but most patients in the e-prescription analysis came from practices using NextGen, while the majority in the med list analysis came from practices using eMDs. Nearly all GC records were for prednisone (90%). In the e-prescription analysis, the median average daily GC dose was higher in EHR data compared to Medicare claims (median (IQR) 3.1 mg (1.4-5.1) vs. 2.5 mg (0.9-4.8)); on the contrary, median average daily dose was lower in EHR med lists compared to Medicare claims (median 2.5 mg (1.2-4.9) vs. 3.0 (1.2-5.2)). In both analyses, 83-88% patients had an EHR average daily GC dose within 5 mg of their Medicare dose; 30-40% were within 1 mg. Accuracy for classifying patients as GC users of particular doses and durations based on EHR data varied from 0.59 to 0.95 but was highest for patients receiving >10 mg prednisone daily for durations > 180 days (Figure).
Conclusion: In this national study, we found discrepancies between GC exposure derived from two sources of EHR data (e-prescription orders and medication lists) and Medicare Part D claims among patients with RA. Caution should be exercised when using EHR data to derive GC exposure over short periods but may be suitable for ascertaining GC exposure at higher daily doses taken for longer periods of time.
To cite this abstract in AMA style:
Li J, Kay J, Abada S, Palmowski A, Stovall R, Yazdany J, Schmajuk G. Uncovering Discrepancies: Analysis of Glucocorticoid Exposure Among Patients with Rheumatoid Arthritis in Electronic Health Record Data versus Medicare Claims [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/uncovering-discrepancies-analysis-of-glucocorticoid-exposure-among-patients-with-rheumatoid-arthritis-in-electronic-health-record-data-versus-medicare-claims/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uncovering-discrepancies-analysis-of-glucocorticoid-exposure-among-patients-with-rheumatoid-arthritis-in-electronic-health-record-data-versus-medicare-claims/