Session Information
Date: Tuesday, November 12, 2019
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
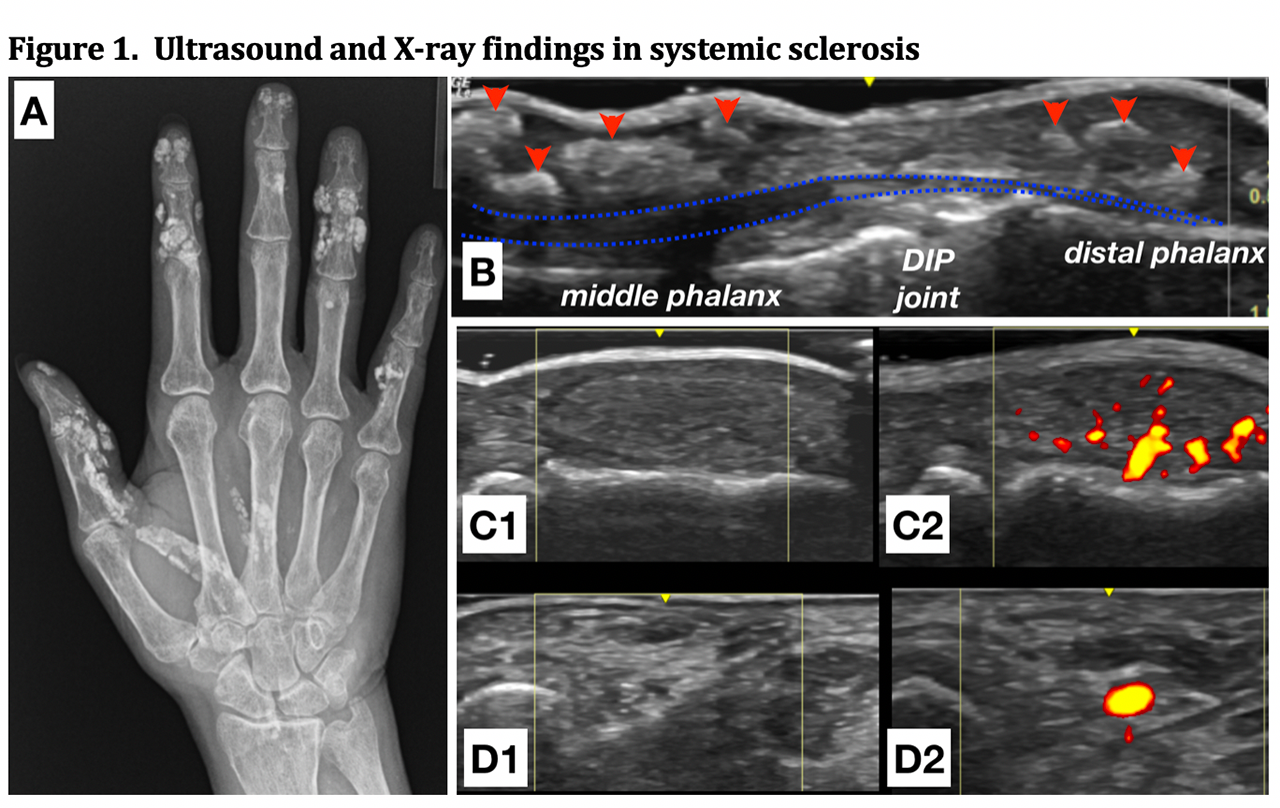
Background/Purpose: Systemic Sclerosis (SSc) is a progressive fibrotic and vascular disease affecting multiple organs. Calcinosis cutis in SSc is characterized by calcium deposition in the skin and subcutaneous tissues and can lead to significant morbidity. While the pathophysiology of calcinosis in SSc is poorly understood, vascular ischemia is thought to play a role. Ultrasound (US) is well suited to vascular and soft tissue interrogation and may be helpful to detect, monitor, and study calcinosis in SSc. We sought to evaluate the ability of US to detect calcinosis in the hands and wrists of SSc patients versus X-ray identified calcinosis and to evaluate the relationship between ultrasound markers of pathologic perfusion and the presence of calcinosis.
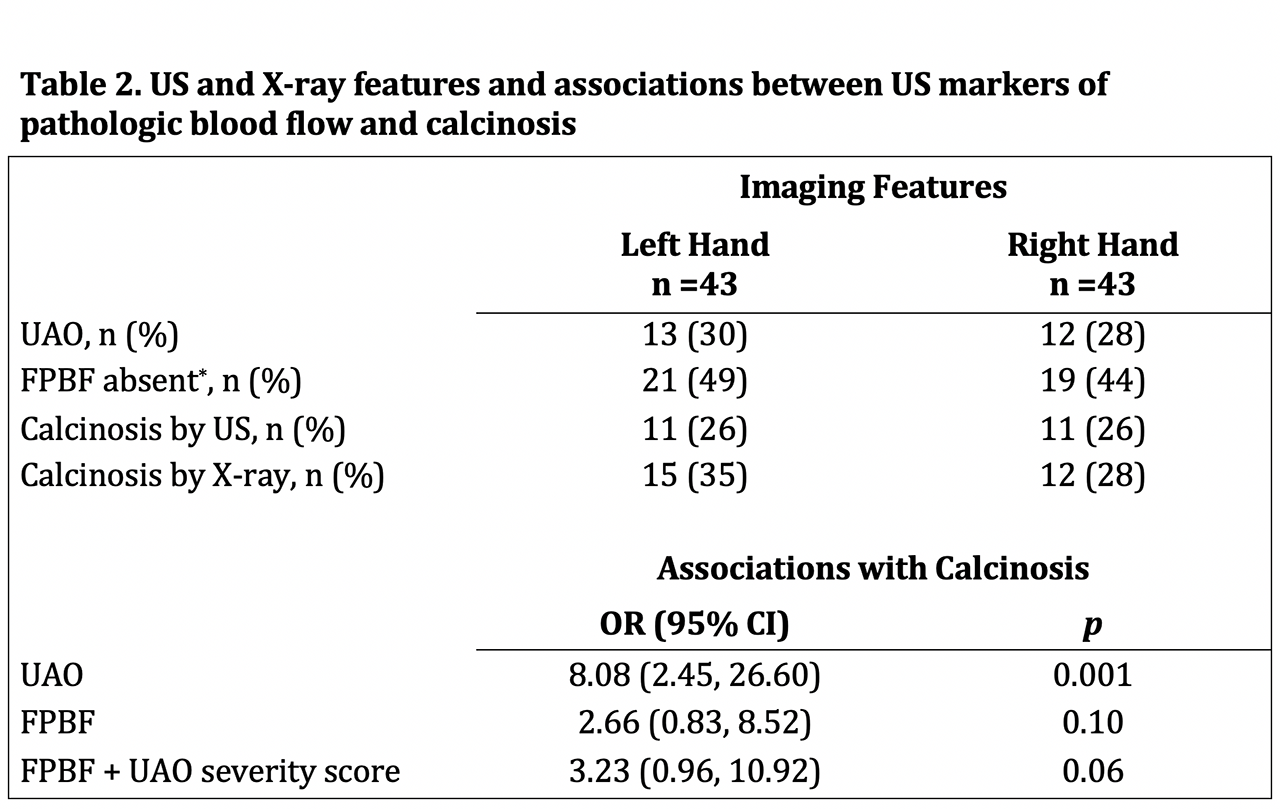
Methods: Patients meeting 2013 ACR/EULAR classification criteria for SSc were prospectively evaluated for calcinosis in the hands and wrists by both X-ray and US. US was performed by submerging the hands and wrists in a water bath for evaluation of all surfaces. The presence or absence of calcinosis was recorded for each of 44 zones (22 left and 22 right) based on our previously published methods, and the sensitivity and specificity for calcinosis detection by US versus X-ray was determined. We also obtained bilateral US vascular measurements of ulnar artery occlusion (UAO) and finger pulp blood flow (FPBF) in the 3rd and 4th digits. For each hand, associations between markers of pathologic blood flow (UAO, FPBF, and a composite severity score of UAO and FPBF) and the presence of calcinosis were assessed using generalized estimating equations.
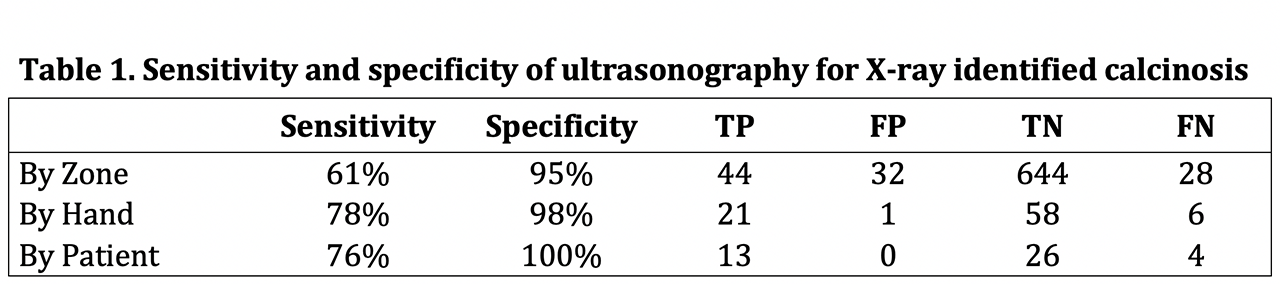
Results: 43 SSc patients (19 diffuse and 24 limited) were enrolled and 17 (39.5%) were found to have X-ray evidence of calcinosis in at least 1 hand (10 bilateral, 7 unilateral). US identified 13 patients with calcinosis (9 bilateral, 4 unilateral). Of the 748 zones evaluated, X-rays identified 72 zones (9.6%) with calcinosis while US showed 76 (10.2%). The sensitivity and specificity for US detection of calcinosis versus X-ray was 61% and 95% by zone, 78% and 98% by hand, and 76% and 100% by patient, respectively. UAO was seen in 13/43 (30%) and 12/43 (28%) of left and right hands, respectively, and FPBF was absent in 1 or both digits of the left and right hands in 21 (49%) and 19 (44%), respectively. We found a strong association between UAO and X-ray identified calcinosis (OR 8.08, 95% CI 2.45-26.60, p< 0.001). Both FPBF (OR 2.66, 95% CI 0.83-8.52, p=0.099) and the composite severity score (OR 3.23, 95% CI 0.96-10.92, p=0.059) failed to show a significant association with calcinosis.
Conclusion: In a cohort of SSc patients we developed a new method for ultrasound detection and quantification of calcinosis and found it to be sensitive, and highly specific versus X-ray. We also found a strong relationship between UAO, a marker of decreased peripheral perfusion, and X-ray identified calcinosis. This is the first study to evaluate the performance of ultrasound in the detection of calcinosis and provides further support for an association between vascular disease in SSc and the pathogenesis of calcinosis.
To cite this abstract in AMA style:
Fairchild R, Chung M, Sharpless L, Li S, Chung L. Ultrasound Detection of Calcinosis and Correlation with Ulnar Artery Occlusion in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/ultrasound-detection-of-calcinosis-and-correlation-with-ulnar-artery-occlusion-in-patients-with-systemic-sclerosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ultrasound-detection-of-calcinosis-and-correlation-with-ulnar-artery-occlusion-in-patients-with-systemic-sclerosis/