Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Recurrent monoarthritis (RM) is a significant therapeutic challenge in rheumatology, often persisting despite NSAIDs, corticosteroids (CS), DMARDs, and biologic therapies. Local interventions like intra-articular aspiration (IAA) and CS injections offer transient relief and are limited by high recurrence rates. Surgical and chemical synovectomy have largely been abandoned due to poor efficacy and high complication rates. Microwave ablation (MWA) is a well-known technique in the treatment of benign or malign lesions of different etiologies. Building upon our initial findings using MWA in RM sucessfully, we present long-term outcomes from a larger cohort of medical treatment-resistant RM, providing real-world data on the efficacy and safety of MWA.
Methods: Patients with RM associated with various inflammatory diseases were included. MWA was performed after measuring the size of synovial hypertrophy (SH) with 15 or 20-watt power and different durations until microbubbles were shown indicating necrosis (Figure 1). Both clinical and radiologic data were recorded baseline and prospectively.
Results: We applied MWA to a total of 43 knee joints in 37 patients (18 female and 19 male) aged between 22 and 71 years. The median number of IAA required in the 6 months prior to MWA was 5 (0–15). Three patients had previously undergone surgical synovectomy. In 3 knees of 2 patients, the number of IAAs in the last 6 months was 0; these patients had persistent synovial effusion and abundant synovial hypertrophy but declined IAA. A 2nd MWA session was required in 5 patients, and 1 patient underwent a 3rd. The median follow-up period was 15 months (5–25). The IAA frequency dropped dramatically from 207 over 258 patient-months (0.81/month) before MWA to just 21 over 624 patient-months post-MWA (0.03/month; p < 0.001). Short-term, Lowe dose CS therapy was administered in 14 patients (16 knees) with all anti-inflammatory treatments maintained unchanged during the first 6 months post-procedure. CS reduction or cessation was achieved in 16 patients. Functional disability and pain scores showed significant improvement, with the median score decreasing from 9 to 1 (p < 0.0001 for both, Figure 2). No complications were observed during the procedure or follow-up. While both SH and effusion persisted to varying degrees at the 1st and 3rd months on USG and MRI, IAA was deferred unless symptoms developed. Significant regression in SH was demonstrated on MRI at the 6th month (Figure 3). A discordance between clinical improvement and radiological findings was observed in a small subset of the cohort.
Conclusion: MWA is a safe, effective, and minimally invasive adjunctive option for managing RM with SH. It significantly reduces arthritis flares frequency, CS dependecy, and the need for IAAs while improving functional outcomes and pain. Although early imaging may show persistent effusion and SH, significant regression by six months correlates with sustained clinical improvements. These long-term results support MWA as a promising alternative to surgical interventions in RM resistant to conventional medical therapies.
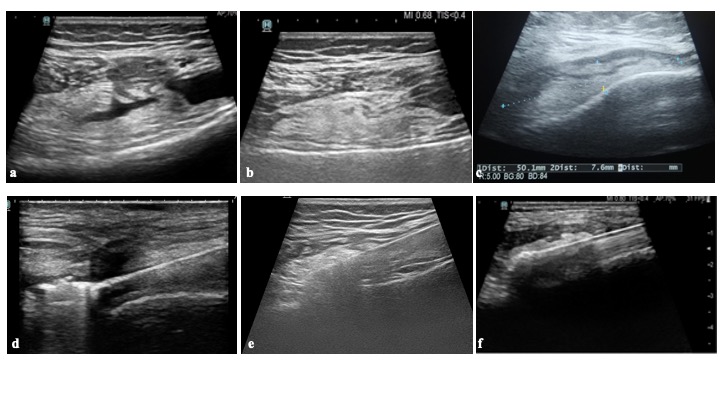 Figure 1. Microwave Ablation Technique. Synovial hypertrophy was assessed using ultrasound (USG), and significant joint effusion, if present, was aspirated. The targeted hypertrophic area is demonstrated in panels 1a and 1b, and the measurement of horizontal and longitudinal dimensions is shown in panel 1c. Following surgical asepsis and local anesthesia, antimicrobial prophylaxis with ampicillin/sulbactam and sedation with midazolam and fentanyl were administered. A monopolar internally cooled MWA probe was inserted through a 2 mm skin incision under USG guidance. Examples of probe placement into hypertrophic synovium are illustrated in panels 1d, 1e, and 1f. Ablation was performed using 15–20 W of energy with the moving-shot technique until microbubbles, indicating effective necrosis, were observed (panels 1d and 1f). For larger hypertrophic areas, multiple ablation zones were treated sequentially. Energy output and ablation duration were recorded.
Figure 1. Microwave Ablation Technique. Synovial hypertrophy was assessed using ultrasound (USG), and significant joint effusion, if present, was aspirated. The targeted hypertrophic area is demonstrated in panels 1a and 1b, and the measurement of horizontal and longitudinal dimensions is shown in panel 1c. Following surgical asepsis and local anesthesia, antimicrobial prophylaxis with ampicillin/sulbactam and sedation with midazolam and fentanyl were administered. A monopolar internally cooled MWA probe was inserted through a 2 mm skin incision under USG guidance. Examples of probe placement into hypertrophic synovium are illustrated in panels 1d, 1e, and 1f. Ablation was performed using 15–20 W of energy with the moving-shot technique until microbubbles, indicating effective necrosis, were observed (panels 1d and 1f). For larger hypertrophic areas, multiple ablation zones were treated sequentially. Energy output and ablation duration were recorded.
.jpg) Figure 2: Functional disability and pain scores of patients before MWA procedure and at 1st, 3rd, 6th, and 12th month visits. The figure 2a shows the functional disability score and 2b shows the pain score rated between 0 an 10. 0 means no funcitonal disability or pain, and 10 is the worst possible funcitonal disability or pain, in both.
Figure 2: Functional disability and pain scores of patients before MWA procedure and at 1st, 3rd, 6th, and 12th month visits. The figure 2a shows the functional disability score and 2b shows the pain score rated between 0 an 10. 0 means no funcitonal disability or pain, and 10 is the worst possible funcitonal disability or pain, in both.
.jpg) Figure 3: An example of a patient with pre-procedure, and post-procedure 1st, 3rd, 6th, and 12th month MRI images indicating consistent improvement in MRI findings with time. The figure 3a shows pre-procedure, 3b shows post-procedure 1st month, 3c shows post-procedure 3rd month, 3d shows post-procedure 6th month, and 3e shows post-procedure 12th month MR images of the patients. In all rows, the order of images are positron density weighted (PDW) in the axial plane, PDW in the sagittal plane, T1-weighted contrast enhanced in the axial plane, and T1-weighted contrast enhanced in the sagittial plane, from left to right. Synovial hypertrophy and effusion did not show any significant change in the 1st and 3rd months after the procedure, whereas a significant regression was observed starting from the 6th month.
Figure 3: An example of a patient with pre-procedure, and post-procedure 1st, 3rd, 6th, and 12th month MRI images indicating consistent improvement in MRI findings with time. The figure 3a shows pre-procedure, 3b shows post-procedure 1st month, 3c shows post-procedure 3rd month, 3d shows post-procedure 6th month, and 3e shows post-procedure 12th month MR images of the patients. In all rows, the order of images are positron density weighted (PDW) in the axial plane, PDW in the sagittal plane, T1-weighted contrast enhanced in the axial plane, and T1-weighted contrast enhanced in the sagittial plane, from left to right. Synovial hypertrophy and effusion did not show any significant change in the 1st and 3rd months after the procedure, whereas a significant regression was observed starting from the 6th month.
To cite this abstract in AMA style:
Deniz R, Güzelbey T, Mutlu İ, Kalkan K, Kılıçkesmez Ö, Bes C. Two-Year Outcomes of Microwave Ablation for Recurrent Monoarthritis with Synovial Hypertrophy Resistant to Medical Treatment: Expanded Cohort and Long-Term Follow-Up Results [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/two-year-outcomes-of-microwave-ablation-for-recurrent-monoarthritis-with-synovial-hypertrophy-resistant-to-medical-treatment-expanded-cohort-and-long-term-follow-up-results/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/two-year-outcomes-of-microwave-ablation-for-recurrent-monoarthritis-with-synovial-hypertrophy-resistant-to-medical-treatment-expanded-cohort-and-long-term-follow-up-results/
