Session Information
Date: Sunday, November 8, 2020
Title: Pediatric Rheumatology – Clinical Poster II: Systemic JIA, Autoinflammatory, & Scleroderma
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: To compare bone lesion evolution and bone lesion distribution patterns identified by whole body magnetic resonance imaging (WB-MRI) by treatment intensity in patients with chronic recurrent multifocal osteomyelitis (CRMO).
Methods: We performed an IRB-approved observational study of previously collected data from a large longitudinal CRMO cohort at the University of Iowa. We extracted detailed demographic, clinical, treatment and imaging data in patients with biopsy-proven CRMO who have undergone ≥2 serial WB-MRIs between 2014-2019. WB-MRIs were reviewed by two pediatric radiologists with expertise in imaging of CRMO. Bone lesions were characterized for anatomic location and lesion evolution on serial scans; specifically, we identified the total number of unique lesions on initial and follow-up scans, as well as fully resolved lesions at the final scan. We stratified our CRMO cohort into four treatment groups based on a hierarchical therapy approach reflective of clinical practice at our institution. We defined the active treatment groups at the time of the initial WB-MRI scan. The four groups were: non-steroidal anti-inflammatory (NSAID) group (defined as active NSAID use only); synthetic disease-modifying antirheumatic drug (DMARD) group (defined as active sDMARD ± NSAID); biological DMARD group (defined as active bDMARD ± sDMARD ± NSAID); and bisphosphonate group (defined as active bisphosphonate use ± bDMARD ± sDMARD ± NSAID). Descriptive statistics were used to compare the 4 treatment intensity groups.
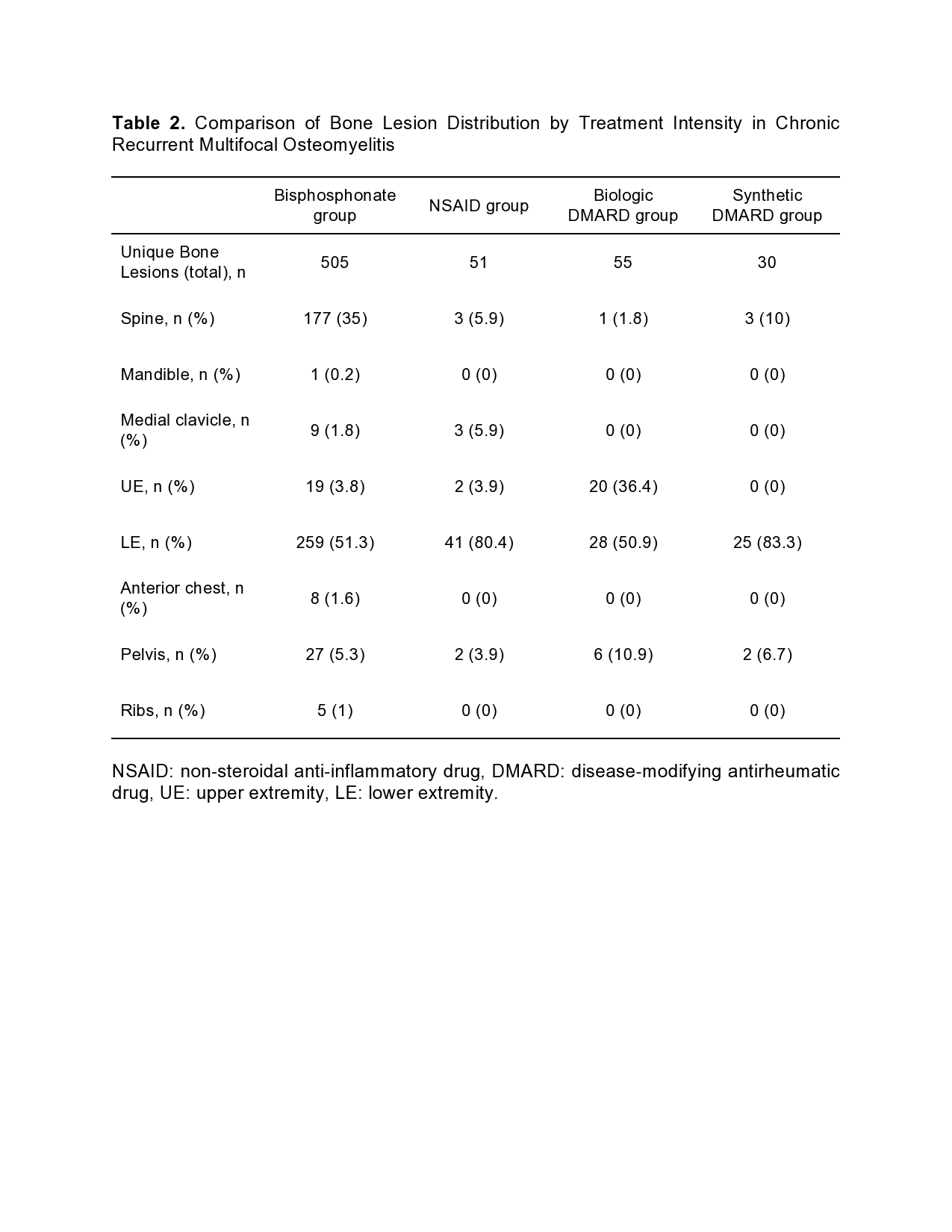
Results: The findings of our study are summarized in Tables 1 and 2. In our CRMO cohort (n=51), the majority of patients belonged to the bisphosphonate group (n=28), followed by NSAID (n=10), bDMARD (n=8) and sDMARD (n=5) groups respectively (Table 1). Mean age, sex distribution and mean follow-up time were overall similar across groups, except for younger age and higher proportion of females in the sDMARD group. Prior systemic glucocorticoid use was similar, except less frequent in the NSAID group. Patients in the bisphosphonate group had the highest total and mean (per patient) number of bone lesions identified on WB-MRI (Table 1). Additionally, the mean number of bone lesions per patient was ~4x higher on initial and ~8x higher on follow-up imaging in the bisphosphonate group compared to the three non-bisphosphonate groups. The bone lesion distribution pattern in the bisphosphonate group most frequently involved the lower extremity (LE), spine and pelvis; this group had the highest spine burden compared to other groups (Table 2). Peripheral (upper extremity and LE), medial clavicular and pelvic bone lesions, without spine involvement, were a common pattern observed in the NSAID, bDMARD and sDMARD groups. The proportion of resolved bone lesions on follow-up imaging was highest in the bisphosphonate group, followed by bDMARD group.
Conclusion: Treatment-stratified bone lesion evolution and distribution patterns reflect the severity of CRMO and current management strategies. Further study to elucidate differential treatment effects on individual bone lesions is needed to individualize therapeutic approaches in patients with severe CRMO.
To cite this abstract in AMA style:
Lenert A, Sato T, Kandemirli S, Ten Eyck P, Ferguson P. Treatment Intensity and Impact on Bone Lesion Evolution and Distribution Patterns in Severe Chronic Recurrent Multifocal Osteomyelitis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/treatment-intensity-and-impact-on-bone-lesion-evolution-and-distribution-patterns-in-severe-chronic-recurrent-multifocal-osteomyelitis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-intensity-and-impact-on-bone-lesion-evolution-and-distribution-patterns-in-severe-chronic-recurrent-multifocal-osteomyelitis/