Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiopulmonary complications are the number one cause of mortality in Systemic sclerosis (SSc). We studied the prevalence, cumulative incidence, predictors and impact of interstitial lung disease (ILD) on survival in a recent inception cohort of SSc patients.
Methods: A comprehensive retrospective review of individual medical records was done to assemble a population-based cohort of incident SSc patients from January 1, 2010, through December 31, 2020, who were followed until death, migration from the geographic area, or September 30, 2022. ILD at baseline was identified on high-resolution CT scan, and cumulative incidence of ILD adjusting for competing risk of death was estimated. Cox models were used to examine risk factors for ILD and its time-dependent impact on survival.
Results: We identified 146 incident SSc patients (81% F, 90% Caucasian, mean age = 59.5 ± 13.6 y, mean follow-up 4.8 ± 3.1 y) over the 11-y period. Majority had limited cutaneous SSc (122), followed by diffuse cutaneous SSc (18), and SSc sine scleroderma (6). Anti-nuclear antibody (ANA) was positive in 94% of (134/143) patients, anticentromere in 53% (77/144), anti-Scl 70 in 11% (16/146), and anti-RNA polymerase III in 18% (25/142). Of 146 patients, 19 (13%) had ILD prior to SSc diagnosis, and 29 (out of remaining 127) developed ILD during follow-up. The cumulative incidence of ILD in SSc (excluding 19 cases with ILD prior to index date) was highest in the initial few years after diagnosis of SSc with 13.4% (95% CI 8.6%-21.0%) at 1 y, 21.9% (95% CI 15.3%-31.3%) at 5 y, and 28.7% (95% CI 20.5-40.3%) at 10 y. Overall, the cumulative incidence of ILD in SSc (including 19 cases with ILD prior to index date was 24.7% (95% CI 18.6-32.8%) at 1 y, 32.1% (95% CI 24.9-41.2%) at 5 y, and 38.0% (95% CI 29.8-48.6%) at 10 y. (Figure 1)
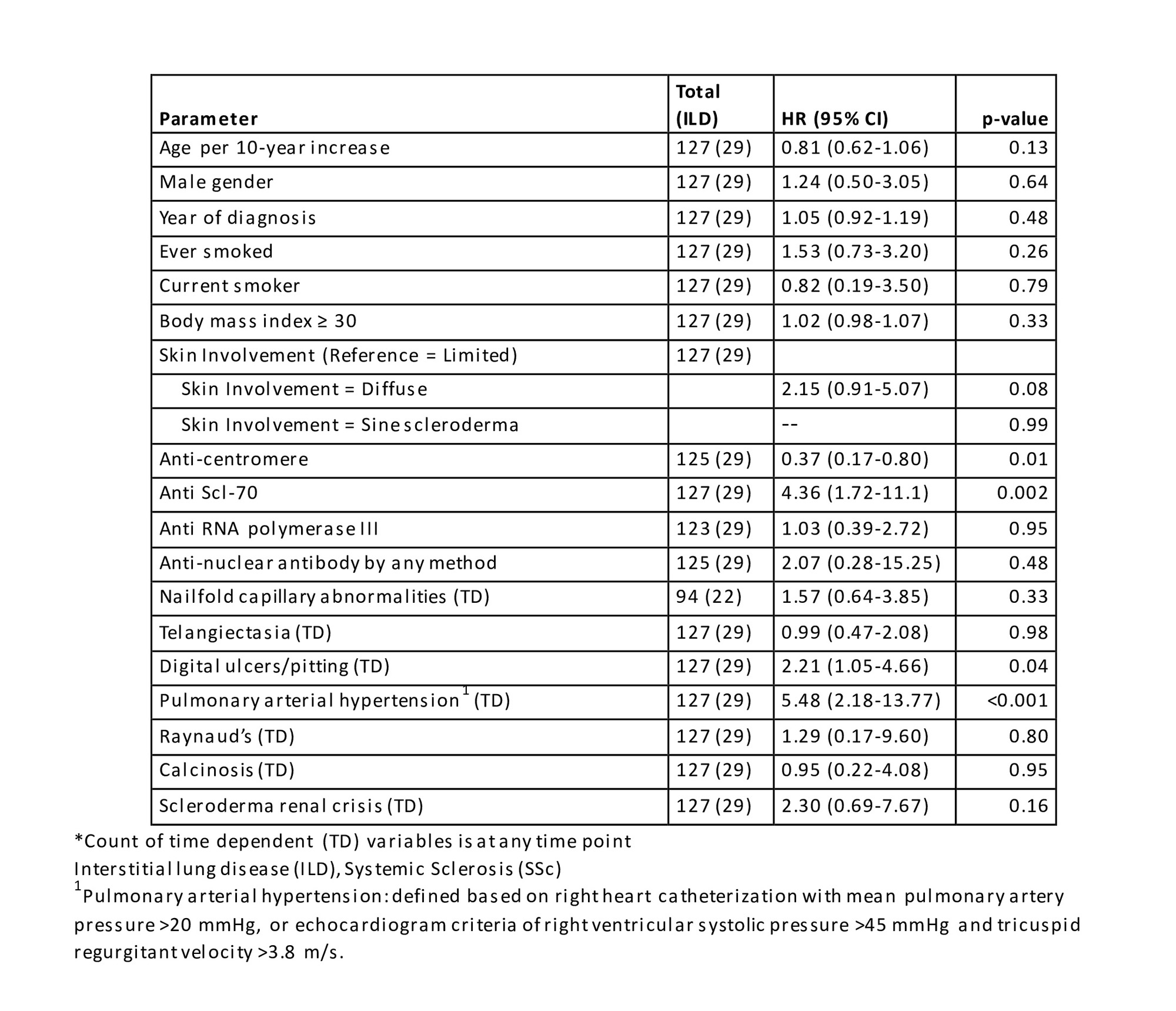
Age, gender, and smoking did not affect the risk for the development of ILD in patients with SSc. A higher risk was associated with digital ulcers/pitting (HR 2.21, 95% CI 1.05-4.66; p=0.04) and a trend towards higher risk with diffuse skin involvement (HR 2.15, 95% CI 0.91-5.07; p=0.08). Anti-centromere antibody was a protective factor (HR 0.37, 95% CI 0.17-0.80; p=0.01), while anti-Scl 70 strongly increased the risk for ILD (HR 4.36, 95% CI 1.72-11.1; p=0.002). Pulmonary arterial hypertension (PAH) was also associated with a significantly increased risk of ILD (HR 5.48; 95%CI 2.18-13.77). (Table 1)
ILD increased the risk of overall mortality in patients with SSc (HR 3.65, 95% CI 1.72-7.71 adjusted for age, sex and index year). This higher but non-statistically significant risk persisted after adjusting for age, sex, and PAH (as a time-dependent variable) (HR 1.96, 95% CI 0.89-4.33).
Conclusion: ILD is a common visceral complication of SSc and a major contributor to morbidity and mortality in these patients. While it is known to be a complication of ‘early’ disease, a substantial portion of patients continue to develop ILD between 5-10 years after disease onset. ILD confers a nearly 4-fold higher risk of overall mortality in SSc patients, which may be complicated by co-existing PAH. These findings highlight the importance of thorough pulmonary evaluation not only at diagnosis and in the early years of disease but also during long-term follow-up in SSc patients.
To cite this abstract in AMA style:
Karn A, Achenbach S, Hinze A, Crowson C, Makol A. Time Trends, Cumulative Incidence, and Impact on Survival of Interstitial Lung Disease in Systemic Sclerosis: Results from a Population-based Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/time-trends-cumulative-incidence-and-impact-on-survival-of-interstitial-lung-disease-in-systemic-sclerosis-results-from-a-population-based-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/time-trends-cumulative-incidence-and-impact-on-survival-of-interstitial-lung-disease-in-systemic-sclerosis-results-from-a-population-based-cohort-study/