Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Some antidepressants and anticonvulsants are effective in treating pain through mechanisms thought to be independent from their effects on depression, such as tricyclic antidepressants (TCAs) (such as amitriptyline), serotonin-norepinephrine reuptake inhibitors (SNRIs) (such as duloxetine), and gabapentinoids (GBPs, anticonvulsant also used off-label for depression). In contrast, selective serotonin reuptake inhibitors (SSRIs) (such as fluoxetine), are first-line agents for managing depression but their analgesic effects are unclear. Whether agents that predominantly ameliorate depression, which adversely affects the pain experience, can positively impact knee osteoarthritis (OA) is not clear. We aimed to evaluate the relation of the use of analgesic antidepressants (AAD, including TCAs, SNRIs, and GBPs) compared with SSRIs to the risk of knee/hip replacement among people with OA in a population-based cohort.
Methods: We conducted a propensity score-matched, new-user design, active comparator, population-based cohort study using data from IQVIA Medical Record Database (IMRD from January 1, 2000, to December 31, 2021, limited to people with prevalent OA age 40-89. We excluded participants with rheumatoid arthritis and common contraindications to joint replacement. From among this OA sample, we identified incident AAD and SSRI users, and propensity-score matched them 1:1 using one-year cohort accrual blocks. We compared the risk of knee/hip replacement among AAD initiators to SSRI initiators using Cox proportional hazards regression. Participants were followed from the date of initial AAD or SSRI prescription until the first of any of the following: the occurrence of the outcome, death, transfer out of the GP practice, the last data collection date by the GP, when a participant reached the age of 90, or the end of study on December 31, 2021. We conducted subgroup analyses by further limiting participant with OA and depression. We repeated analyses accounting for the competing risk of death using a Fine-Gray model.
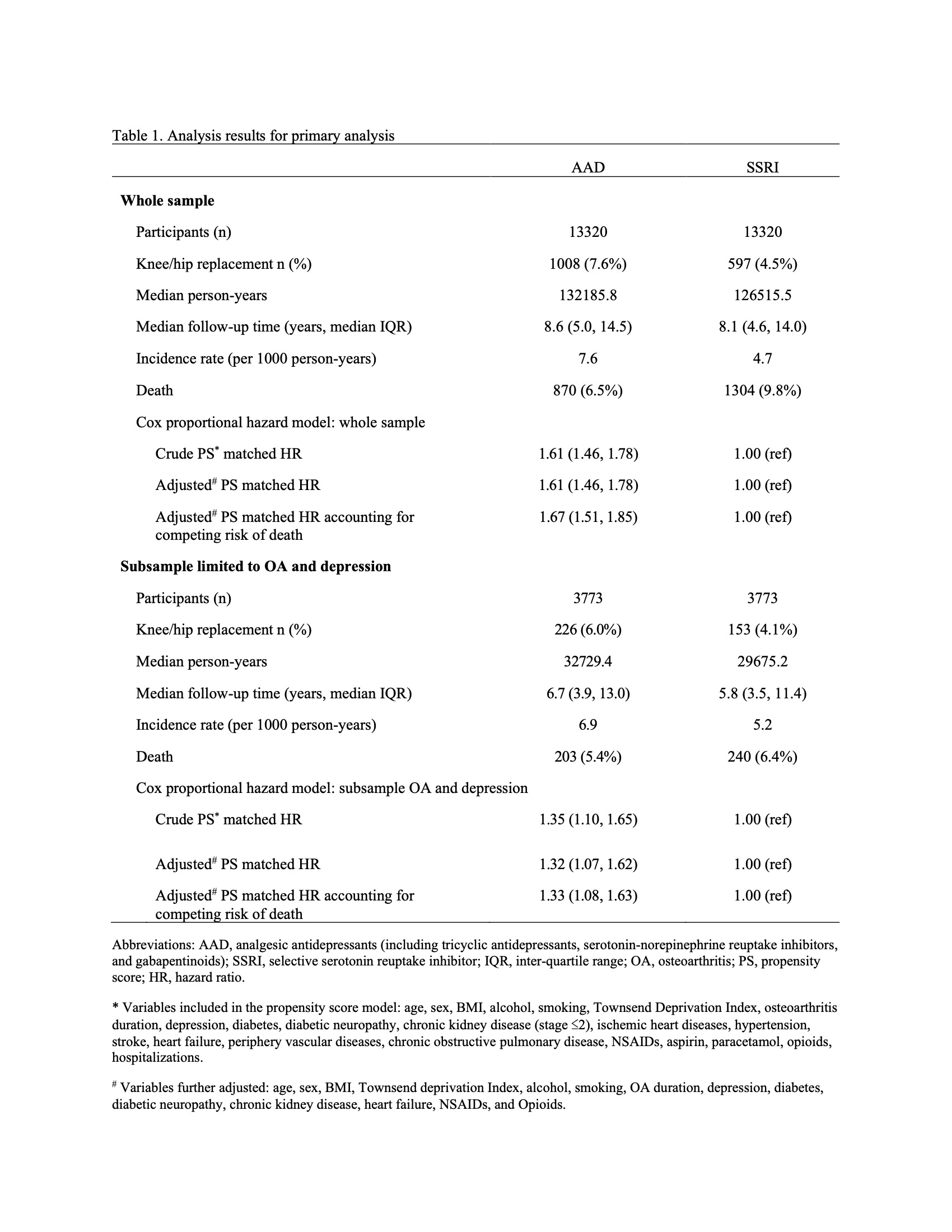
Results: Of the 13320 initiators of AAD (mean age 67, 63% female) and 13320 initiators of SSRI (mean age 67, 64% female), 1008 (7.6%) and 597 (4.5%), respectively, had a knee/hip replacement with a median follow-up time of 8.6 and 8.1 years, respectively.
Initiators of AAD had a higher risk of knee/hip replacement compared with initiators of SSRI, with the propensity score–matched hazard ratio (HR) of 1.61 (95% CI 1.46, 1.78). When additionally adjusted for confounders and when accounting for competing risk of death, the effect estimates remained similar (HR 1.61; 95% CI 1.46, 1.78) and (HR 1.67; 95% CI 1.51, 1.85), respectively. (Table 1). Subgroup analyses limited to participants with OA and depression showed smaller effect estimates.
Conclusion: AAD initiation was associated with a higher risk of knee/hip replacement compared with SSRI initiation. These results may reflect confounding by indication and/or may suggest that agents that predominantly impact depression may also have beneficial symptom effects in knee OA.
To cite this abstract in AMA style:
Wang Z, Westerland M, Peloquin C, LaValley m, Clancy M, Ding C, Neogi T. The Relations of Analgesic Antidepressants Use to Knee or Hip Replacement Among Osteoarthritis Patients Compared to Selective Serotonin Reuptake Inhibitors in a Large Prospective Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-relations-of-analgesic-antidepressants-use-to-knee-or-hip-replacement-among-osteoarthritis-patients-compared-to-selective-serotonin-reuptake-inhibitors-in-a-large-prospective-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-relations-of-analgesic-antidepressants-use-to-knee-or-hip-replacement-among-osteoarthritis-patients-compared-to-selective-serotonin-reuptake-inhibitors-in-a-large-prospective-cohort/